Strategies and Approaches for Investigating Patient Safety Events
Shaikh U. Strategies and Approaches for Investigating Patient Safety Events. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2022.
Shaikh U. Strategies and Approaches for Investigating Patient Safety Events. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2022.
Background
This primer provides a broad overview of three widely used tools for investigating and responding to patient safety events and near misses. Tools covered in this primer include incident reporting systems, Root Cause Analysis (RCA), and Failure Modes and Effects Analysis (FMEA). These tools have been used in high-risk industries and occupations such as aviation, manufacturing, nuclear power, and the military and have been adapted for use in enhancing patient safety in healthcare settings over the past two decades.
Incident Reporting Systems
Incident reporting systems are widely used by health care organizations to ascertain and document adverse events or high-risk situations. They are a general term for patient safety event reporting systems where voluntary reports are made by frontline health care staff directly involved in events. Incident reporting systems provide insights into patient harms at the organizational level and can promote shared learning within and across organizations to prevent or reduce risks. In addition to reporting adverse events, reporting of near misses allows organizations to develop strategies to prevent events from occurring.
Incident reports set the stage for the use of other patient safety tools that are then employed to investigate and mitigate safety events. To be maximally effective, incident reporting systems should be coupled with supportive institutional cultures that value patient safety, policies and procedures to ensure the confidentiality of employees who submit reports, encourage submission of reports from a broad range of healthcare professionals, integrate mechanisms to ensure timely review of reports, and close the loop by developing and communicating action plans to individuals who submit reports and other stakeholders.
Incident reporting systems are a form of passive surveillance and therefore have limitations in their ability to provide a comprehensive assessment of patient safety concerns. Moreover, adverse events and near misses in health care are underreported. Barriers to incident reporting include an organizational culture of blame, health care staff's fear of repercussions, and inadequate integration of reports into electronic health records. By celebrating employees who report patient safety hazards and shifting the focus from the number of events reported to system-level changes, organizations can promote a just culture that focuses on learning and psychological safety instead of punishment.
Examples of incident reporting systems used as part of larger efforts to improve patient safety have included initiatives to reduce patient falls, medication errors, and wrong-site and wrong-patient surgical errors.
Root Cause Analysis
Root cause analyses (RCAs) are problem-solving tools and techniques used to retrospectively discover causes of patient safety adverse events and near misses. Root causes are core issues that directly lead to the safety issue. The goal of RCA is to identify root causes, identify corrective actions, and eliminate these root causes through systems-based process improvement approaches.1 A key aspect of RCA is identifying underlying systems-level causes that contribute to patient safety problems, while avoiding blame setting or focusing on individual mistakes.
Variations in RCA techniques lead to variations in the effectiveness of RCAs. The identification and implementation of corrective actions is highly context-dependent, which makes it challenging to measure the true impact of RCAs. Although there is wide variation in how RCA is employed in organizations to improve patient safety, common steps include defining the problem, brainstorming potential causes, understanding causes and effects, and designing one or more solutions to sustainably prevent the issue from recurring.
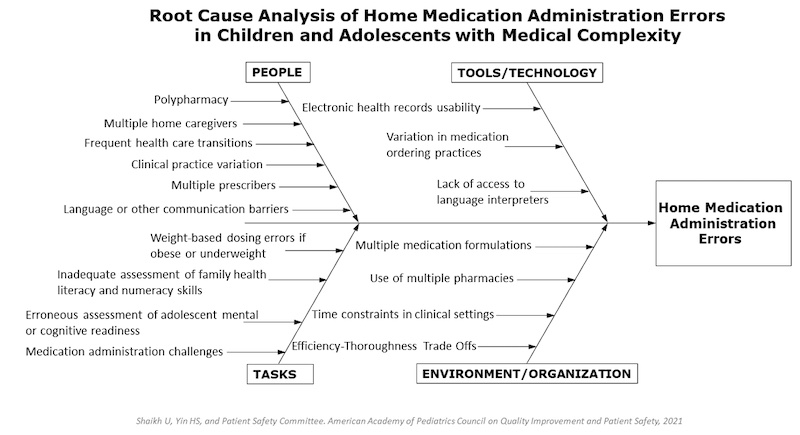
A cause-and-effect diagram, also called a fishbone or Ishikawa diagram, is a helpful visual tool that can be used to conduct an RCA. It is helpful in structuring brainstorming sessions where healthcare teams identify several potential causes of patient safety adverse events or near misses and sort them into categories.2
RCAs are more effective when conducted by a team of people from the process or area where the patient safety issue occurred, who are expected to work together to uncover root causes and to implement solutions to mitigate or eliminate root causes. To be effective, RCAs require an investment of time, resources, organizational commitment, and patient and family engagement to identify and implement a range of corrective actions. The concept of Root Cause Analysis and Action (RCA2) emphasizes that the processes of analyzing and implementing systems-based corrective actions need to go hand in hand to improve patient safety.
Examples where RCA have been used to improve patient safety as part of larger organizational efforts have included identifying reasons for diagnosis and treatment delays, reducing patient falls, preventing wrong-patient or wrong-site errors, addressing device malfunction, and preventing medication errors.
Figure. Example Root Cause Analysis
Failure Modes and Effects Analysis
Failure modes and effects analysis (FMEA) is a structured adverse event analysis tool that aims to prospectively identify potential failures in processes, products, or services. The goal of FMEA is to prioritize failures based on their potential seriousness and to design and implement actions to mitigate or prevent failures in order of priority.
The initial step in an FMEA is to assemble a team of individuals with a range of knowledge and experience about the process, product, or service. The team then conducts detailed process mapping to identify all the steps in the process that is being investigated. One this is done, “failure modes”, i.e., ways in which a process or product could potentially fail or result in a defect or error, are identified. The term “effects analysis” refers to analyzing the consequences of such failures by prioritizing their severity, likelihood of occurrence, and likelihood of detection. A risk priority number, generated using these variables, provides a quantitative estimate of the level of hazard involved in various steps of the process and helps prioritize patient safety efforts. Using this approach, components of the process or product most in need of change are identified, and potential patient safety events are mitigated and prevented.3
Rather than simply reacting to adverse events after they have occurred, FMEA focuses on engaging health care team members in analyzing and modifying processes, products, or services proactively to prevent future adverse events. This approach is ideally used as early as possible and continues throughout the operation of the product or service, thereby continually improving the safety of health care systems for patients and staff.
Examples of use of FMEA to improve patient safety have included transformations in medication delivery processes to prevent medication errors, assessing blood transfusion processes to prevent morbidity and mortality from transfusion errors, and restructuring hospital policies and processes to prevent patient falls.4
Although incident reporting systems, RCA, and FMEA are all key tools for investigating and responding to patient safety events, they do not by themselves result in sustainable improvements in patient safety unless they are used in conjunction with larger systems-level quality improvement efforts.
Ulfat Shaikh, MD, MPH, MS
Associate Editor, AHRQ’s Patient Safety Network (PSNet)
Professor of Pediatrics
Medical Director for Healthcare Quality
UC Davis Health
ushaikh@ucdavis.edu
References
- Oakes D. Root Cause Analysis: The Core of Problem Solving and Corrective Action, Second Edition. ASQ Quality Press; 2019. ISBN: 978-0-87389-982-6.
- Fishbone diagram. ASQ. Accessed March 17, 2022 [Available at]
- How planning for failure can make telehealth safer. Institute for Healthcare Improvement (IHI). Accessed March 17, 2022. [Available at]
- Gowdy M, Godfrey S. Using tools to assess and prevent inpatient falls. Jt Comm J Qual Saf. 2003 Jul;29(7):363-8. [Available at]