Weighing In on Surgical Safety
Brodsky JB, Margarson M. Weighing In on Surgical Safety. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2010.
Brodsky JB, Margarson M. Weighing In on Surgical Safety. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2010.
Case Objectives
- Identify the comorbidites associated with obesity that place patients at higher risk for surgical complications.
- Understand elements of the STOP-BANG questionnaire that help screen patients for obstructive sleep apnea.
- Explain the most effective strategies for managing anesthesia and postoperative pain control in the obese patient.
- Appreciate the role of positioning to ensure safe outcomes for surgical patients with obesity.
Case & Commentary: Part 1
A 54-year-old man with diabetes mellitus, hypertension, and obstructive sleep apnea (OSA) was referred to an orthopedic surgeon after many years of left knee pain. Despite aggressive efforts with physical therapy and medications to treat his pain, the patient continued to experience increasing functional limitations. Although he tried to lose weight many times, his body mass index remained 40 kg/m2 (normal is approximately 19-25). After having a total knee replacement recommended, he was referred to a preoperative clinic for evaluation.
Every day we are bombarded with newspaper, television, and radio headlines reminding us of the worldwide obesity epidemic. Obesity has become a major problem in both industrialized and developing countries. Today in the United States, more than two-thirds of the adult population is overweight (body mass index [BMI] > 25 kg/m2), and more than one-third is obese (BMI > 30 kg/m2). Significant obesity, often termed morbid obesity (BMI > 40 kg/m2), is associated with many medical comorbidities. This patient is typical, suffering from hypertension, type 2 diabetes mellitus, OSA, and osteoarthritis.
In order to reduce perioperative risks, medical comorbidities must be recognized, evaluated, and properly treated if necessary, prior to elective surgery. The presence and degree of obesity influence some of the technical aspects of anesthetic management (e.g., airway intubation, drug distribution and uptake, risk of pressure injury), but poorly controlled medical comorbidities are probably the most important factors increasing the overall risk of morbidity and mortality in this patient population. As a rule, general anesthesia and airway manipulation are best avoided in the extremely obese patient, and regional anesthetic techniques, although technically more challenging, are preferred if practical.
In patients like the one presented, hypertension must be adequately controlled and antihypertensive medications should be continued even on the day of surgery. The one exception is angiotensin-converting enzyme inhibitors, such as lisinopril, which should be stopped before surgery since they can cause marked hypotension on induction of anesthesia. Although the incidence of ischemic heart disease is increased in patients with obesity, a resting ECG is usually sufficient for baseline investigation if the patient has good exercise tolerance and no signs or symptoms of heart disease. The ability to easily climb stairs without dyspnea demonstrates reasonable cardiovascular reserve. However, most morbidly obese patients also have back and knee osteoarthritis, which severely limits physical activity and makes most forms of simple, clinical stress testing impossible. For patients with limited exercise tolerance or difficulty assessing this tolerance, additional evaluation by a cardiologist may be indicated.(1) Often the only clue that a patient suffers from cardiac dysfunction is the presence of orthopnea and fluid retention, usually presenting with pitting edema of the legs. Even modest degrees of ankle edema can suggest right heart failure and pulmonary hypertension in the obese patient.(2) These would all be important screening elements in the history and physical examination when conducting the preoperative evaluation in an obese patient.
Insulin and other diabetic medications should be continued until the day of surgery and then withheld. In diabetic patients, the operation should ideally be scheduled for the morning. Blood sugar should be monitored intraoperatively and throughout the postoperative period, and insulin administered as required. There are existing practice guidelines that assist providers in managing perioperative glycemic control.
Our patient also has a history of OSA. The "STOP" questionnaire is a simple tool that asks about the presence of factors associated with OSA. STOP stands for loud snoring, tiredness during the daytime, observed apneas, and high blood pressure.(3) A further refinement (the "STOP-BANG" questionnaire) includes questions about BMI, age, neck circumference, and male gender. The results of these questionnaires are suggestive but not diagnostic of OSA. A definitive diagnosis of OSA can only be made by polysomnography. However, since there is a very high association between OSA and morbid obesity, it is prudent to consider all such patients as having sleep apnea and to manage them accordingly. Mild to moderate OSA may be asymptomatic and of minor importance, but severe and long-term OSA is associated with chronic hypoxemia, pulmonary and systemic hypertension, and cardiac failure. Untreated chronic OSA can increase operative risk. Nocturnal continuous positive airway pressure (CPAP) therapy should be instituted 4-6 weeks before planned surgery. Patients on CPAP have reductions in both systemic and pulmonary hypertension and experience an improvement in functional capacity. Unfortunately, compliance may be a problem in some patients, and others may not wish to delay surgery. Likewise, weight loss prior to elective surgery is encouraged and may alleviate some comorbidities, but most morbidly obese patients are unable to lose significant weight without bariatric weight loss surgery.
In summary, with the proper preoperative risk reduction strategies, our patient would be a reasonable candidate for surgery, but risks remain because of the discussed comorbidities related to his obesity.
Case & Commentary: Part 2
The patient underwent a preoperative evaluation and, after a discussion about risks and benefits, he consented to a total knee replacement. The plan was to use general anesthesia supplemented by use of an epidural catheter for postoperative pain control. On the day of surgery and in the operating suite, the patient was placed in a supine position for induction of anesthesia. The patient soon experienced hemodynamic instability and hypoxia, and, despite many efforts, providers were unable to establish a functioning airway. The patient soon became pulseless, a code was called, and the patient expired after failed resuscitative attempts.
Normally, combining general and epidural anesthesia is an acceptable plan for any patient undergoing elective knee replacement surgery, although using only an epidural for both intra- and postoperative analgesia may have been a better choice for this morbidly obese patient. A regional anesthetic alone offers many advantages for the obese patient, including minimal need for airway manipulation, reduced use of potentially cardiopulmonary depressing anesthetic agents, and a lower incidence of postoperative nausea and vomiting.(4) An epidural can provide excellent postoperative pain control, thereby lowering opioid requirements, an important consideration for obese patients prone to pulmonary complications. Whichever anesthetic technique is used, sedative premedication should be avoided whenever possible. Many, if not most, morbidly obese patients with OSA are extremely sensitive to the respiratory depressive effects of even small doses of sedatives and opioids.(5)
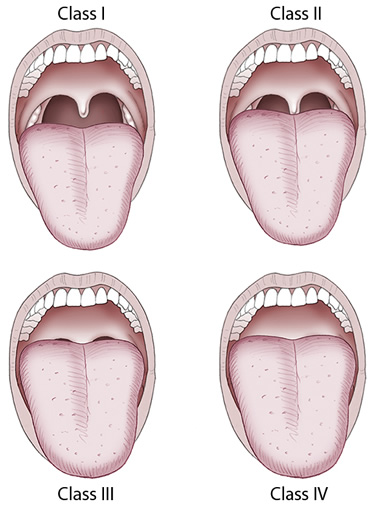
The combination of a large neck circumference (> 40 cm) and high Mallampati score (III-IV) is the best predictor of potential airway intubation difficulties.(6-7) The Mallampati score is used by anesthesiologists to try to predict difficulty with direct laryngoscopy. A Mallampati score of I or II is usually associated with an easy intubation, while scores of III and IV are more predictive of difficulty (Figure 1). For any high-risk patient (and many morbidly obese patients fit into this category), an awake fiberoptic-assisted intubation or use of a video-laryngoscope should be considered. However, for most morbidly obese patients, placement of a tracheal tube by direct laryngoscopy is usually no more problematic than for a normal-weight patient, provided that proper steps are taken to ensure success. An assistant experienced with airway management must always be immediately available should problems occur, since a second pair of hands may be necessary to help with bag-mask ventilation should intubation of the airway fail.
The error in this patient's care that resulted in the tragic outcome was the attempt to induce general anesthesia while he was supine—a known and very real danger in morbidly obese patients. Even when sitting or standing, extremely obese patients have markedly reduced functional residual capacity, and lung volume is further reduced when they lie flat.(8) The supine position causes significant increases in oxygen consumption, cardiac output, and pulmonary artery pressure. Simply lying down leads to a decrease in already poor chest wall compliance, greater perfusion mismatch, and a sudden shift of blood to an already hyperactive, borderline hypoxic heart. In patients with inadequate cardiac reserve, these acute changes can cause fatal cardio-respiratory decompensation, as was demonstrated more than 30 years ago in a report aptly titled "Obesity Supine Death Syndrome."(9) As this case tragically demonstrates, these observations are still not fully appreciated.
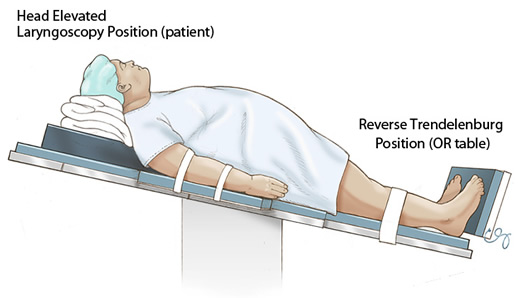
Proper positioning is essential. A head-up position facilitates mask ventilation, improves the laryngoscopist's view during direct laryngoscopy, and most importantly recruits lung volume and increases oxygen reserves.(10) The "head-elevated laryngoscopy position," in which the head and upper body are elevated so that an imaginary horizontal line can be drawn from the sternum to the ear, increases the success of direct laryngoscopy in morbidly obese patients (Figure 2).(11) Head-up positions also increase "safe apnea time" (i.e., the time between pre-oxygenation and muscle paralysis until oxyhemoglobin begins to significantly desaturate). The longer the safe apnea time, the more time available to secure the airway before the patient becomes hypoxemic. Maximum safe apnea time for morbidly obese patients can be achieved with the operating room table in the reverse Trendelenburg position.(12) Therefore, our practice at the start of every case with general anesthetic is to position the extremely obese patient in the head-elevated laryngoscopy position with the operating room table in the reverse Trendelenburg position (Figure 3).
After adequate pre-oxygenation, induction of general anesthesia is performed with intravenous propofol. Opinion is currently divided as to which muscle relaxant is best for tracheal intubation for obese patients—the choice is between the depolarizing relaxant succinylcholine and the non-depolarizing relaxant rocuronium. Although both have a rapid onset and both provide satisfactory conditions, succinylcholine allows for consistently better views during laryngoscopy. Succinylcholine has a short duration of action; should difficulties be encountered, paralysis will wear off within 8-10 minutes and the patient will resume spontaneous breathing. If rocuronium is used and difficulties occur (as in this case), its neuromuscular blocking effects must be reversed or the patient will remain paralyzed for a much longer period. Although the drug sugammadex does have the ability to reverse rocuronium immediately, it is not yet available in the United States. Until sugammadex becomes available, we recommend succinylcholine for tracheal intubation of obese patients.
If the trachea is not successfully intubated and mask ventilation becomes "impossible" (as occurred in this case), placement of a laryngeal mask airway and changing from the supine to reverse Trendelenburg position may be enough to allow adequate oxygenation. However, if the vocal cords have been traumatized from unsuccessful attempts at tracheal intubation, a surgical airway may be the only option. Unfortunately, cricothyroidotomy or tracheostomy in a morbidly obese patient with a large neck is not easily or rapidly achieved.
The obesity epidemic means that every anesthesia and surgical care provider will see more and more extremely obese patients in their daily practice. With proper preparation, monitoring, and an awareness of their unique needs and challenges, morbidly obese patients can safely undergo any surgical procedure. A completed plan, perhaps even a checklist, should be prepared prior to anesthetizing an extremely obese patient. To guide management, each case should begin with a list of each medical comorbidity and what steps have been taken to optimize that condition. An airway management decision tree should also be considered. Once the decision is made to access the airway, a list of what steps and what equipment should be available to maintain adequate ventilation (similar to the American Society of Anesthesiologists "Difficult Airway Algorithm") if the initial plans to intubate the trachea fail. For each patient, calculation of various weight formulas (BMI, lean body weight, and ideal body weight) prior to administering any drugs will avoid under- or overdosage since various agents are given based on these different weights.
Given the number of obese patients currently undergoing surgery, and the predicted increase in that number in the future, every anesthesia training program should place an emphasis on teaching the principles of management of these patients. The morbidly obese patient presents a complex clinical challenge, and continuous ongoing medical education and keeping current with the latest strategies for the care of the obese patient are necessary.(13) This case had a devastating outcome, one that probably could have been avoided if the anesthesia provider had been familiar with the management of the obese patient.
Take-Home Points
- Since morbid obesity is associated with so many medical comorbidities, including hypertension, cardiovascular disease, type 2 diabetes, OSA, and osteoarthritis, preoperative evaluation is essential to recognize these medical and physiologic changes in order to optimize pre-existing conditions.
- The STOP-BANG questionnaire helps identify the presence of OSA. In the absence of a definitive diagnosis, which is made by polysomnography, all morbidly obese patients should be treated as if they have OSA.
- Minimize or avoid sedatives and opioids during the entire perioperative period.
- A sedated morbidly obese patient should never lie supine. For induction of general anesthesia, always ensure proper positioning to maximize oxygen reserves.
- Whenever practical, chose a regional anesthetic and avoid general anesthesia and tracheal intubation.
Jay B. Brodsky, MD Professor (Anesthesia) Medical Director, Perioperative Services
Stanford University Medical Center
Michael Margarson, MD Department of Anaesthesia St. Richard's Hospital
Chichester, UK
Faculty Disclosure: Dr. Brodsky and Dr. Margarson declare that they have no financial arrangements or other relationship with the manufacturers of any commercial products discussed in this continuing education activity. In addition, their commentary does not include information regarding investigational or off-label use of pharmaceutical products or medical devices.
References
1. Poirier P, Alpert MA, Fleisher LA, et al. Cardiovascular evaluation and management of severely obese patients undergoing surgery: a science advisory from the American Heart Association. Circulation. 2009;120:86-95. [go to PubMed]
2. O'Hearn DJ, Gold AR, Gold MS, Diggs P, Scharf SM. Lower extremity edema and pulmonary hypertension in morbidly obese patients with obstructive sleep apnea. Sleep Breath. 2009:13:25-34. [go to PubMed]
3. Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology. 2008;108:812-821. [go to PubMed]
4. Ingrande J, Brodsky JB, Lemmens HJ. Regional anesthesia and obesity. Curr Opin Anaesthesiol. 2009;22:683-686. [go to PubMed]
5. Candiotti K, Sharma S, Shankar S. Obesity, obstructive sleep apnoea, and diabetes mellitus: anesthetic implications. Br J Anaesth. 2009;(suppl 103):i23-i30. [go to PubMed]
6. Brodsky JB, Lemmens HJM, Brock-Utne JG, Vierra M, Saidman LJ. Morbid obesity and tracheal intubation. Anesth Analg. 2002;94:732-736. [go to PubMed]
7. Neligan PJ, Porter S, Max B, Malhotra G, Greenblatt EP, Ochroch EA. Obstructive sleep apnea is not a risk factor for difficult intubation in morbidly obese patients. Anesth Analg. 2009;109:1182-1186. [go to PubMed]
8. Biring MS, Lewis MI, Liu JI, Mohsenifar Z. Pulmonary physiologic changes of morbid obesity. Am J Med Soc. 1999;318:293-297. [go to PubMed]
9. Tsueda K, Debrand M, Zeok SS, Wright BD, Griffin WO. Obesity supine death syndrome: reports of two morbidly obese patients. Anesth Analg. 1979;58:345-347. [go to PubMed]
10. Perilli V, Sollazzi L, Bozza P, et al. The effects of the reverse Trendelenburg position on respiratory mechanics and blood gases in morbidly obese patients during bariatric surgery. Anesth Analg. 2000;91:1520-1525. [go to PubMed]
11. Collins JS, Lemmens HJ, Brodsky JB, Brock-Utne JG, Levitan RM. Laryngoscopy and morbid obesity: a comparison of the "sniff" and "ramped" positions. Obes Surg. 2004;14:1171-1175. [go to PubMed]
12. Boyce JR, Ness T, Castroman P, Gleysteen JJ. A preliminary study of the optimal anesthesia positioning for the morbidly obese patient. Obes Surg. 2003;13:4-9. [go to PubMed]
13. Alavarez A, Brodsky JB, Lemmens HJM, Morton JM, eds. Morbid Obesity: Peri-operative Management. 2nd edition. Cambridge, UK: Cambridge University Press; 2010. ISBN: 9780521518840.
Figures
Figure 1. Determining Mallampati scores.
Figure 2. Head-elevated laryngoscopy position.
Figure 3. Patient positioned in head-elevated laryngoscopy position with the operating room table in the reverse Trendelenburg position. (Illustration © 2010 Chris Gralapp.)