Point-of-care Mixup: 1 Shot Turns Into 3
Berberich RF. Point-of-care Mixup: 1 Shot Turns Into 3. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2017.
Berberich RF. Point-of-care Mixup: 1 Shot Turns Into 3. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2017.
The Case
A 2-month-old boy was brought in for a routine 2-month well-child visit. The exam was completed and the appropriate vaccinations were ordered, including Pentacel (which contains vaccines against DTaP [diphtheria, tetanus, pertussis], Hib [Haemophilis influenza], IPV [inactivated polio vaccine]), Hep B (hepatitis B), PCV (pneumococcal conjugate vaccine), and RV (rotavirus). The nurse gave the vaccinations to the infant, and then, when documenting them in the electronic health record, noticed she had given the DTaP vaccination, not the Pentacel combination. The patient and his mother were still in the exam room; the mother was breastfeeding the infant.
The physician spoke with the mother about the error. The mother was distressed to learn that her son would need two additional injections but agreed for them to be given because she knew her child needed the additional vaccinations (Hib and IPV). The patient cried and was difficult to settle after the additional injections. In the postincident review, the nurse described being rushed and because of that, she did not properly verify the vaccinations against the orders before administering them.
The Commentary
by F. Ralph Berberich, MD
Childhood immunization ranks highest among the most significant life-saving pediatric public health achievements of our era. The benefit of complete and timely immunization is scientifically indisputable.(1) Current vaccination schedules take into account age-related immunogenicity, the periods of maximum risk from the illnesses against which each vaccine protects, illness severity, the benefits of herd immunity, untoward reactions and adverse effects, and the comparable effectiveness of multiple-component combined vaccines.(2,3) For example, in order to fully protect an infant against whooping cough, an initial immunization at age 2 months, followed by 2 booster injections, each 2 months apart, are required.(2) The morbidity and mortality associated with this illness in children under 1 year of age is dramatic in comparison to that experienced by older children. Adverse effects are few and not age dependent, making it both illogical and dangerous to delay the timing of first dose or booster intervals.(4)
Unfortunately, despite this proven effectiveness, there remains a sense of parental uneasiness about the immunization process.(5) Doubt and suspicion often color, and even disrupt, evidence-supported practice. Part of the concern likely stems from the more than 25 separate injections associated with the required vaccination schedule for children up to the age of 5. Despite the advent of combination vaccines, children experience pain and parents fear adverse effects at virtually every well-child primary health care visit, from infancy to school age. The accretion of shots is remembered by child and parent alike (6) and this has contributed to anti-vaccination movements, solicitation of illegitimate exemptions, the need for public health legislation, and efforts to promote so-called selective vaccines (also known as delayed or single vaccines), or other alternative circumventing schedules.(4)
Part of the concern of parents, even those who appreciate the strong evidence behind vaccination, is pain on injection. The impact of injection pain has not received as much attention in the pediatric literature as it deserves.(7,8) Yet there has been progress in reducing immunization pain in infancy (1,9) and later in childhood.(10) Among the effective methods are the administration of 24% sucrose, non-nutritive sucking or breast feeding, positioning on the lap, discontinuation of syringe aspiration, and warming of the syringe prior to injection.(9) Older children benefit from behavioral and distraction interventions.(10) Attention to providing comfort and reducing pain can do much to make the immunization experience less distressing.
In the case presented, a two-injection routine vaccination recommended by the Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices expanded to five because of an administration error and a delay of the first two hepatitis B immunizations. This caused distress for the infant and the mother, even though the doctor explained how it came about and probably reassured the parent that immunogenicity would be unimpaired. We do not know whether the impact of pain was discussed, either preceding immunizations or as another consequence of the error. We must assume that the vaccines and their potential side effects were reviewed with the mother before administration and the CDC Vaccination Information Sheets handed out as required by law.
Adverse events following immunization are tracked by a number of agencies.(11) The Vaccine Errors Reporting Program (VERP) of the Institute for Safe Medication Practices (monitors those that come to its attention. The Clinical Immunization Safety Assessment Network, a collaborative effort between the CDC and seven academic medical centers, promotes research and safety assessment, although it is not specific to errors in administration. The Vaccine Adverse Event Reporting System database includes immunization errors.
Mistakes can occur in all medical settings. In this case, the nurse's error owed, at least in part, to a systemic problem of vaccine management within the practice. Omission of verification suggests that a deeper problem may exist. Many parts of the immunization process can lead to error; these include transportation, storage, identification, expiration date, confusion over trade names and packaging, mixing with diluent, dosage, timing after reconstitution, immunization scheduling, intramuscular versus subcutaneous, administration technique, and documentation. In order to prevent future errors, the proper recording of the vaccine, date, and lot number are vital. The schedules, exceptions, and catch-up strategies are sufficiently complex so as to require systematic checking and rechecking to avoid mistakes.(12) Where there is uncertainty, advice line services can improve the accuracy and quality of immunization practice.(13)
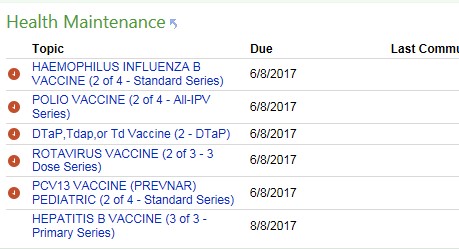
While system problems are the dominant ones, human error can also be at play. In a recent extensive analysis of more than 600 outpatient pediatric vaccination error reports, look-alike and sound-alike confusion accounted for a disproportionate number of wrong vaccine errors.(14) Wrong time errors tended to occur far more with scheduled vaccines than with seasonal or intermittent ones such as influenza. Wrong route and wrong patient mistakes were relatively rare. Human factors challenges played a significant role.(14) Increasing use of electronic health records and template-driven order sets may reduce such errors, but they are only as helpful as the clinician and vaccine administrator's ability to work with them accurately.(15) The best computer provider order entry (CPOE) systems are those that incorporate and hardwire predetermined schedules, doses, and metrics that must be satisfied with order sets that reduce the human error potential (Figure). Yet, when it comes to accuracy, improper prior immunization entry, selection of the wrong age "Smart Set" templates, and hidden errors in vaccine preparation can thwart the best intentions. Providing workflows that satisfy all the redundancies and checks required to ensure safety will vary from institution to institution. Whether as part of student training, or as a matter of periodic review, learning programs covering all aspects of vaccine administration safety are essential. The World Health Organization Vaccine Safety Basics e-learning course is a fine example with international applicability. The immunization core of pediatric well-child health care deserves extraordinary precision and accuracy to maintain its primacy.
Take-Home Points
- Accurate and timely immunizations are a vital component of childhood well care.
- The reduction of immunization pain deserves attention as it is yet another potential source of vaccine hesitancy.
- Strict adherence to published vaccine protocols that ensure safety, efficacy, comfort, and error prevention must be inviolate.
- Redundant crosschecks along each step from procurement to administration offer the best protection against inadvertent errors.
F. Ralph Berberich, MD Pediatrics, East Bay Physicians Medical Group Berkeley, CA
References
1. Offit PA, Moser CA. Vaccines and Your Child: Separating Fact From Fiction. New York, NY: Columbia University Press; 2011. ISBN: 978023115307.
2. Chatterjee A, O'Keefe C, Varman M, et al. Comparative immunogenicity and safety of different multivalent component pertussis vaccine formulations and a 5-component acellular pertussis vaccine in infants and toddlers: a randomized, controlled, open-label, multicenter study. Vaccine. 2012;30:3360-3368. [go to PubMed]
3. Hansen J, Timbol J, Lewis N, et al. Safety of DTaP-IPV/Hib vaccine administered routinely to infants and toddlers. Vaccine. 2016;34:4172-4179. [go to PubMed]
4. Offit PA, Moser CA. The problem with Dr. Bob's Alternative Vaccine Schedule. Pediatrics. 2009:123;e164-e169. [go to PubMed]
5. Wheeler M, Buttenheim AM. Parental vaccine concerns, information source, and choice of alternative immunization schedules. Hum Vaccin Immunother. 2013;9:1782-1789. [go to PubMed]
6. Noel M, McMurtry CM, Pavlova M, Taddio A. Brief clinical report: a systematic review and meta-analysis of pain memory-reframing interventions for children's needle procedures. Pain Pract. 2018;18:123-129. [go to PubMed]
7. Berberich FR, Schechter NL. Pediatric office pain: crying for attention. Pediatrics. 2012;129:e1057-e1059. [go to PubMed]
8. Taddio A, Chambers CT, Halperin SA, et al. Inadequate pain management during childhood immunizations: the nerve of it. Clin Ther. 2009;31(suppl 2):S152-S167. [Available at]
9. Taddio A, McMurtry CM, Shah V, et al; HELPinKids&Adults. Reducing pain during vaccine injections: clinical practice guideline. CMAJ. 2015;187:975-982. [go to PubMed]
10. Berberich FR, Landman Z. Reducing immunization discomfort in 4- to 6- year old children: a randomized clinical trial. Pediatrics. 2009;124:e203-e209. [go to PubMed]
11. Miller ER, Shimabukuro TT, Hibbs BF, Moro PL, Broder KR, Vellozzi C. Vaccine safety resources for nurses. Am J Nurs. 2015;115:55-58. [go to PubMed]
12. Maurer W. The importance of precise documentation of vaccination by physicians and vaccine providers. Curr Drug Saf. 2015;10:27-30. [go to PubMed]
13. Strohfus PK, Brown SR, Potratz P. Effective and sustainable advice line promotes safe vaccine practices. Int J Evid Based Health. 2016;14:130-135. [go to PubMed]
14. Bundy DG, Shore AD, Morlock LL, Miller MR. Pediatric vaccination errors: application of the "5 rights" framework to a national error reporting database. Vaccine. 2009;27:3890-3896. [go to PubMed]
15. Rogers J, Sebastian S, Cotton W, Pippin C, Merandi J. Reduction of immunization errors through practitioner education and addition of age-specific alerts in the electronic prescribing system. Am J Health Sys Pharm. 2016;73(11 suppl 3);S74-S79. [go to PubMed]