Empty Handoff
The Case
A 29-year-old man with "brittle diabetes" was admitted to the surgery service for incision and drainage of a leg wound. The patient's medical history included chronic renal failure, hypertension, and prior stroke after a hypoglycemia event. Prior to surgery while still on the hospital floor, the patient's blood glucose level fell precipitously after receiving insulin, requiring glucose several times. Due to workload, the nurse did not accompany the patient during transport to the operating room (OR). Instead, the nurse informed the transportation assistant about the patient's extreme sensitivity to insulin.
The transportation assistant neglected to pass this information on to the surgical nurse or the anesthesiologist. The electronic health record (EHR) did not reflect the glucose levels because the bedside glucose-monitoring device was not docked, so the information did not upload to the EHR for physician or nurse review. The patient spent 90 minutes in surgery and went to the recovery room where the blood sugar level was found to be 15 mg/dL, confirmed on repeat testing. Fortunately, the patient recovered quickly once he received intravenous glucose.
The Commentary
It is not difficult to put oneself in the position of the senior nurse in a busy surgical ward trying to juggle the tradeoff of getting patients through the system while keeping a balance on patient safety. Then, at that moment, add to the mix a complex patient with brittle diabetes, a labile blood glucose, chronic renal failure, and previous stroke who the operating team is now calling for. This scenario will test a safety system to the limit.
Overwhelmed by the tasks at hand, the ward nurse sees her only option as to ask the transportation assistant to pass on one bit of vital patient information to the operating room team. Now, put yourself in the shoes of the transportation assistant, who is not clinically trained and who also has a list of tasks to accomplish. Not surprisingly, the assistant simply forgets to mention the glucose issue when he drops off the patient.
In the face of growing needs to get more surgical patients through busy systems while keeping patients safe, it is vital to create robust, reliable systems for patient handoffs. This case clearly illustrates the futility of relying on individuals, even careful and well meaning ones, to bridge these gaps.
Communication failures are commonly cited as the most frequent causes of medical error, and handoffs are particularly vulnerable. In a study of 60 surgical malpractice claims associated with poor communication, 43% involved poor handoffs (equating to about 10% of all surgical injury malpractice claims).(1) In a more recent study, 59% of residents reported that, during their most recent rotation, they had harmed one or more patients as a result of handoff-related errors, with about 1 in 5 reporting major harm.(2) However, errors that do not lead to harm are far more frequent, with most cases involving some form of information transfer error.(3) Handoffs in surgical care often involve equipment transfers, which may carry higher risk, but for which there is less easily derived evidence. The workload associated with simultaneous handoff of information, equipment, and physical transfer between care teams of different specialties (anesthesia, surgery, nursing, intensive care) further increases the chances of errors, with the potential for compounding errors particularly insidious. The capacity of handoff errors to remain undetected for significant periods of time—as illustrated by this case—further compounds this risk. Thus, the consequences of errors associated with handoffs can be diverse and may be difficult to identify. With increased specialization and reductions in trainee work hours, first in Europe and more recently the United States, the number of care transitions is increasing, which means the potential for these types of errors is also increasing.
In 2006, The Joint Commission issued National Patient Safety Goal 2E which requires a "standardized approach to handoff communications, including an opportunity to ask and respond to questions." Perhaps the most ubiquitous attempt to standardize handoffs has been the SBAR (situation, background, assessment, and recommendation) mnemonic.(4) Also prevalent have been checklist-type interventions, where information exchange is standardized through structured documentation.(5) However, both approaches are limited single-dimension considerations, addressing only one aspect of handoff (e.g., communication, teamwork, process standardization, or information management), while other important aspects can remain unaddressed (e.g., distractions, equipment, workspace, training, planning, decision-making, follow-up). Moreover, there are innumerable types of handoffs and little understanding of what "standardization" might be, as their social, teaching, and error-capturing functions especially are difficult to quantify or standardize.(6) In the case study, a high workload led to an unusual secondary handoff to an assistant, which compounded by poor integration of technology and workflow led to an omission prior to surgery that was fortuitously captured. This error chain illustrates the complexity of surgical work, and why uni-dimensional approaches to error avoidance in handoffs are unlikely to be wholly effective.
Despite an enormous growth in handoff research, with more than 200 papers published on this topic in 2010 alone, we still struggle to know what makes an effective handoff. Modeling and multivariate measurement of handoffs is still relatively primitive, and associations between handoff practice and outcomes are extremely difficult to demonstrate. For example, the observed mismatch between perceptions and objective assessments of handover quality suggests that even handoffs that we think are effective can have substantial information omissions.(7) Manser and colleagues (8) identified, through principle component analysis, three key factors that affect quality: information transfer, shared understanding, and working atmosphere. Our own observational study in pediatric cardiac surgery (9), which has subsequently informed and been replicated in adult surgery (10), modeled information errors, equipment errors, and teamwork. The multifactorial and interacting nature of the variables within both models suggests complexity, but also elements of predictability. For example, in changing the handoff process, we demonstrated that a standardized process is less reliant on teamwork to avoid errors than a non-standardized one. However, we also found that the highest degrees of safety are achieved when both standard practices and high levels of teamwork are combined.
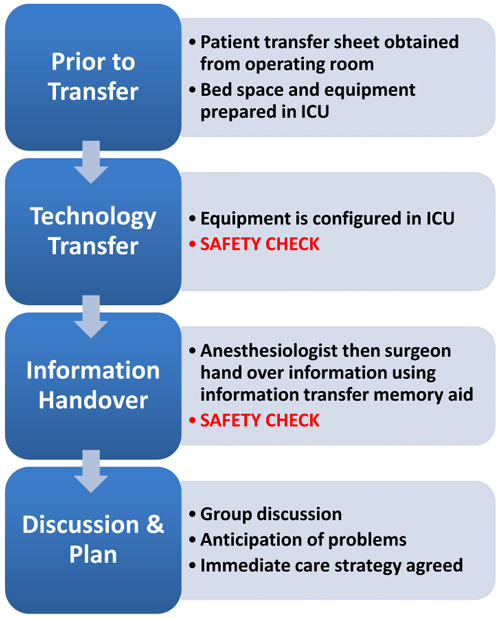
Just as the success of a handoff must be considered along multiple dimensions, so should improvements. Although the idea of a "simple checklist" is attractive, successful change requires considerably more than the production of pieces of paper. In this respect, learning from other industries can be both instructive and inspirational.(11) Despite very clear contextual differences, every complex system aims for improvement, and translating lessons from other systems into health care may yield powerful insights. An overarching lesson is that a substantial part of human work involves making tradeoffs, for example, between safety and efficiency or risk and reward; that procedures or checks evolve over time for necessary human and organizational reasons; and that high performing teams often communicate less frequently, but more effectively.(12) To explore these issues, we studied what OR and intensive care unit (ICU) teams could learn from pit stop crews (Table).(9) In our study, we separated the handoff into four phases. In phase 1, the transferring team (in our study, the operating team) sends a form to the ICU informing them when the patient will be arriving and what equipment and settings are needed. In phase 2, the patient is transported to the unit and technology is transferred in silence (unless any member is concerned about any safety issues with the patient) with each member knowing their role. In phase 3, the team forms a huddle for the handover of patient information, using a standardized format that is guided by a memory aid (the receiving team uses this as part of their admission note, thus incorporating the template into the flow of their work). The receiving team reads back key information handed over. Finally, in phase 4, the whole team (referring and receiving) agrees on a patient plan and contingencies if things go wrong. It is simple and effective.
Our work with pit stop crews illustrated a range of key learning points that may be translated into different types of handoffs. We found that our method—which involves a clear process division between handoff preparation, equipment transfer, information transfer, and discussion, coupled with practical training, safety checks, and documentation integrated with the forward planning and execution of care—led to significant performance improvements that have now been replicated by others (Table and Figure).(10,13) The performance gains included less process errors and information omissions; the impact on patient outcomes was not measured. Given the dynamic nature of most handoff situations, a defense-in-depth strategy might also be worthy of consideration, where, rather than being reliant on the single handoff process itself, errors might be captured using formalized post hoc checks of expectation mismatch (e.g., a patient is sicker than was anticipated), clinical mismatch (e.g., a different condition or diagnosis from what was handed over), or documentation mismatches (e.g., different date of birth, name, history).(14) Though it is clear that many practitioners already do these types of post-handoff checks, this practice is not formalized and is far from ubiquitous. In the case study, this follow-up testing is ultimately what prevented the patient from experiencing significant harm. Finally, continual review and improvement, based on new standards, studies, or local events, is a growing part of health care practice.
Take-Home Points
- Errors in handoffs are frequent; most do not lead to harm, but some can be extremely harmful, with a wide variety of effects.
- Handoffs are multifaceted, complex, dynamic, and sometimes challenging to define and measure. Equipment, information, environment, teamwork, and shared understanding are among the key components of successful handoffs.
- Standardization is possible and desirable, but standardization alone will not yield substantial and sustainable improvements, especially when the standardized component focuses only on a single dimension (e.g., information transfer alone). Standardization should take into consideration: preparation for handover, technology transfer, information transfer using checklist and standardized communication, and a joint plan developed by the multiprofessional teams involved in the handoff.
- The ability to detect, avoid, and manage errors should be considered in any design of a handoff process. Interventions should be multifaceted, resilient, and offer defense-in-depth (i.e., utilize multiple strategies for error capture before, during, and after the formal handoff process).
- The long-term challenge is to maintain a reliable system in ever increasingly busy clinical settings.
Allan Goldman, MB Pediatric Intensivist Clinical Unit Chair for Cardiorespiratory Services Great Ormond Street Hospital
Ken Catchpole, PhD Director of Surgical Safety and Human Factors Research Department of Surgery Cedars-Sinai Medical Center
References
1. Greenberg CC, Regenbogen SE, Studdert DM, et al. Patterns of communication breakdowns resulting in injury to surgical patients. J Am Coll Surg. 2007;204:533-540. [go to PubMed]
2. Kitch BT, Cooper JB, Zapol WM, et al. Handoffs causing patient harm: a survey of medical and surgical house staff. Jt Comm J Qual Patient Saf. 2008;34:563-570. [go to PubMed]
3. Nagpal K, Vats A, Ahmed K, Vincent C, Moorthy K. An evaluation of information transfer through the continuum of surgical care: a feasibility study. Ann Surg. 2010;252:402-407. [go to PubMed]
4. Telem DA, Buch KE, Ellis S, Coakley B, Divino CM. Integration of a formalized handoff system into the surgical curriculum: resident perspectives and early results. Arch Surg. 2011;146:89-93. [go to PubMed]
5. Petrovic MA, Martinez EA, Aboumatar H. Implementing a perioperative handoff tool to improve postprocedural patient transfers. Jt Comm J Qual Patient Saf. 2012;38:135-142. [go to PubMed]
6. Cohen MD, Hilligoss PB. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Qual Saf Health Care. 2010;19:493-497. [go to PubMed]
7. Manser T. Minding the gaps: moving handover research forward. Eur J Anaesthesiol. 2011;28:613-615. [go to PubMed]
8. Manser T, Foster S, Gisin S, Jaeckel D, Ummenhofer W. Assessing the quality of patient handoffs at care transitions. Qual Saf Health Care. 2010;19:e44. [go to PubMed]
9. Catchpole KR, de Leval MR, McEwan A, et al. Patient handover from surgery to intensive care: using Formula 1 pit-stop and aviation models to improve safety and quality. Paediatr Anaesth. 2007;17:470-478. [go to PubMed]
10. Nagpal K, Abboudi M, Fischler L, et al. Evaluation of postoperative handover using a tool to assess information transfer and teamwork. Ann Surg. 2011;253:831-837. [go to PubMed]
11. Patterson ES, Roth EM, Woods DD, Chow R, Gomes JO. Handoff strategies in settings with high consequences for failure: lessons for health care operations. Int J Qual Health Care. 2004;16:125-132. [go to PubMed]
12. Patterson ES. Structuring flexibility: the potential good, bad and ugly in standardisation of handovers. Qual Saf Health Care. 2008;17:4-5. [go to PubMed]
13. Petrovic MA, Aboumatar H, Baumgartner WA, et al. Pilot implementation of a perioperative protocol to guide operating room-to-intensive care unit patient handoffs. J Cardiothorac Vasc Anesth. 2012;26:11-16. [go to PubMed]
14. Thomas MJ, Schultz TJ, Hannaford N, Runciman WB. Failures in transition: learning from incidents relating to clinical handover in acute care. J Healthc Qual. 2013;35:49-56. [go to PubMed]
Table
Table. Applying Pit Stop Practices to Patient Handover Processes.
| Applying Pit Stop Practices to Patient Handover Processes | |||
|---|---|---|---|
| Construct | Pit Stop Practice | Principle | Handover implementation |
| Process Organization | A clear rhythm and order to events | Task sequence |
|
| All team members have clearly defined tasks and roles | Task allocation |
|
|
| Explicit communication strategies to ensure calm and organized atmosphere | Discipline and composure |
|
|
| Teamwork | Leader is the "lollipop man" who has final go/no go decision | Who is in charge? |
|
| Extensive meetings at all levels before every race to establish shared situational picture and goals | Briefings |
|
|
| All team members encouraged to contribute ("it's not about having the best people but having people who work together") | Involvement |
|
|
| Threat & Error Management | Reliability established in safe cultures through extensive documented reminders | Checklists |
|
| Anticipation of weaknesses and having contingencies | Predicting and planning |
|
|
| Overview and error capture by most able team member ("lollipop man"), who notices, understands, and predicts consequences | Situation awareness | Consultants maintain overall picture and awareness by standing back and monitoring rather than being involved in minor tasks |
Figure
Figure. Applying Pit Stop Practices to Patient Handover Processes.