Not a Miscarriage
The Case
A 32-year-old woman, gravida 3, para 1, with a history of Type 2 diabetes mellitus on metformin, presented at 7 and 2/7 weeks by last menstrual period (LMP). The patient reported a history of a primary low transverse cesarean section and a bicornuate uterus. Formal ultrasound revealed an intrauterine gestational sac, with no embryo, and a bicornuate uterus. Beta hCG was 1009 mIU/ml. Hgb A1C was 9.4 g/dL. Her metformin was discontinued and insulin was started.
She was scheduled for a repeat scan approximately 48 hours later, when her hCG would be expected to be over 2000 mIU/ml. At that time, she was spotting, and instead presented to the gynecology clinic. She was seen by an intern who presented the case to an attending and mentioned that the patient had already been found to have an intrauterine pregnancy (IUP) on formal sonogram, but failed to mention her history of a bicornuate uterus. They performed a transvaginal ultrasound, found an empty uterus with a thin stripe, and diagnosed the patient as having a completed spontaneous abortion. At that time, they restarted her metformin.
Several weeks later, the patient went to the family planning clinic for follow-up on a Friday afternoon, at which time a urine pregnancy test was positive. An hCG was checked and found to be 40,000 mIU/ml. She was given a lab slip to return on Monday (before the results were back), as it was unclear whether the urine pregnancy test was positive from an ongoing pregnancy or if she was pregnant again. Her hCG increased, and she was again seen in the gynecology clinic that day, where an ultrasound confirmed a 13 and 3/7 week IUP in the right uterine horn. The patient was then admitted for insulin therapy.
The Commentary
In the case at hand, several important systems failed and a patient with a continuing and desired pregnancy was counseled that she had undergone a spontaneous abortion. The failure to recognize a continuing pregnancy could have led to teratogenic exposure to the fetus. Fortunately, this patient was taking only one medication, metformin, which is pregnancy category B and is not known to be associated with specific adverse consequences. Delayed prenatal care could have resulted in a failure to screen this patient for conditions other than diabetes that might complicate pregnancy and to provide counseling on nutrition and dietary modifications in pregnancy. Before describing systems that could have prevented this error, I will first provide a brief background on Mullerian anomalies, early pregnancy ultrasound, and the evaluation of first-trimester bleeding.
Mullerian Anomalies and Pregnancy
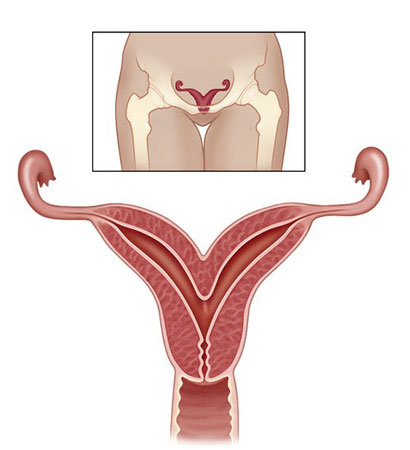
The exact rate of Mullerian anomalies is unknown, as those achieving clinical detection are merely a subset of the most severe phenotypes. The most common is a bicornuate uterus (Figure 1), which is caused by incomplete fusion of the bilateral Mullerian systems during embryogenesis. Having a bicornuate uterus is associated with pregnancy complications including midtrimester pregnancy loss, preterm birth, and malpresentation.(1)
The Role of Ultrasound in Early Pregnancy
Ultrasound is commonly used in the first trimester to assess gestational age. In many circumstances, it provides more accurate dating information than the last menstrual period.(2) In symptomatic or at risk patients, ultrasound can help distinguish spontaneous abortion from ectopic pregnancy. When no intrauterine pregnancy is visualized and no embryo is seen outside of the uterus, a single or serial measurement of the beta subunit of human chorionic gonadotropin (hCG) may be combined with ultrasound to diagnose an abnormal pregnancy of undetermined location, followed by uterine aspiration to make a definitive diagnosis.(3)
In this case, an intrauterine gestational sac was demonstrated on the first ultrasound performed (Figure 2). Therefore, no hCG surveillance was indicated to evaluate the possibility of ectopic pregnancy. Nevertheless, some physicians consider hCG patterns to be valuable in distinguishing normal from abnormal intrauterine pregnancies. Plateauing or declining patterns may prompt early intervention (uterine aspiration) in symptomatic patients.
Classifying Pregnancies with First-Trimester Bleeding
Two classification systems permit us to reliably categorize patients with first-trimester bleeding. The clinical system relies on the pattern of bleeding and pain, uterine size, whether the cervix is open or closed, and (if open) whether tissue is present or not. Putting these data together permits a diagnosis of threatened, inevitable, incomplete, completed, or missed spontaneous abortion. Sonographic classification relies on the sequential appearance of the gestational sac, yolk sac, embryo, and cardiac activity. When thresholds in the normal sequence are breached, a diagnosis of anembryonic pregnancy or early embryonic demise can be made, irrespective of the patient’s symptoms. These two classifications systems are often used together when assessing patients with first trimester bleeding or pain.(4)
Strategies for Minimizing Diagnostic Errors
Several important systems interventions could have prevented the failure to diagnose a continuing pregnancy in this patient.
Optimizing communication of important clinical information.
Until patients are equipped with an electronic summary of their lifetime clinical record stored on portable media, health care providers and institutions will need to be vigilant in their communication, especially when records from one visit are not available at the follow-up visit. Diagnosing and treating ectopic pregnancy prior to catastrophic tubal rupture is so important that many obstetricians keep meticulous information on each patient with first trimester bleeding unless and until an intrauterine pregnancy is visualized on ultrasound or passed at the time of miscarriage.
In this patient, an intrauterine pregnancy was visualized at the initial ultrasound assessment. The patient was not followed with the same vigilance as she would have been if a potentially life-threatening ectopic pregnancy was still a possibility. When the patient presented with spotting, a repeat ultrasound examination was performed in the gynecology clinic. The gynecologist had received an incomplete report on the first ultrasound’s findings from a resident caring for the patient because the official report was not yet available. The resident and the patient did not mention her history of a bicornuate uterus. Had there been an ultrasound report available, this history would have been readily apparent and the repeat ultrasound could have been directed to the uterine horn in which the gestational sac had been detected. In this case, failure of communication and proper sign out from one physician to the other increased the risk of an incomplete ultrasound evaluation.
Relying on systematic checklists when ultrasound studies are performed, regardless of the circumstances or operator.
Radiologists, gynecologists, and other health care providers credentialed in ultrasound assessment may perform these procedures skillfully. Examiner experience is one predictor of diagnostic accuracy.(5) However, errors can be minimized by the routine use of checklists and meticulous documentation of findings, no matter how experienced the operator.(6) The American Institute of Ultrasound in Medicine and the American College of Obstetricians and Gynecologists provide standards and guidelines for obstetrical ultrasound reports. Unfortunately, radiologists and obstetrician/ gynecologists demonstrate similarly low adherence rates to these guidelines in some settings.(7)
The repeat ultrasound on this patient was a limited study assessing the progress of the intrauterine pregnancy noted previously. It appears unlikely that a procedural checklist was used. Such checklists may be developed even for studies of limited focus and purpose, to ensure that they are systematically performed. An “empty uterus” was seen. A complete assessment, including the adnexa, would have substantially reduced the risk of not finding the pregnancy in the other uterine horn.
While it is true that this error would probably have been averted if the patient had reminded the team of her bicornuate uterus, several important safety nets also failed. The failure to diagnose a continuing pregnancy in this patient could have been prevented by ensuring complete communication of the relevant history (lifetime clinical record, physician-to-physician sign-out), the timely availability of new clinical information (ultrasound report), and the routine use of systematic procedural checklists for first-trimester ultrasound.
Lee A. Learman, MD, PhD
Associate Professor and Residency Program Director
UCSF Department of Obstetrics, Gynecology & Reproductive Sciences
Director, General Competencies, UCSF Office of Graduate Medical Education
References
1. Ludmir J, Samuels P, Brooks S, Mennuti MT. Pregnancy outcome of patients with uncorrected uterine anomalies managed in a high-risk obstetric setting. Obstet Gynecol. 1990;75:906-910.[ go to PubMed ]
2. Savitz DA, Terry JW Jr, Dole N, Thorp JM Jr, Siega-Riz AM, Herring AH. Comparison of pregnancy dating by last menstrual period, ultrasound scanning, and their combination. Am J Obstet Gynecol. 2002;187:1660-6.[ go to PubMed ]
3. Barnhart KT, Katz I, Hummel A, Gracia CR. Presumed diagnosis of ectopic pregnancy. Obstet Gynecol. 2002;100:505-10.[ go to PubMed ]
4. Luise C, Jermy K, May C, Costello G, Collins WP, Bourne TH. Outcome of expectant management of spontaneous first trimester miscarriage: observational study. BMJ. 2002;324:873-5.[ go to PubMed ]
5. Wojak JC, Clayton MJ, Nolan TE. Outcomes of ultrasound diagnosis of ectopic pregnancy. Dependence on observer experience. Invest Radiol. 1995;30:115-7.[ go to PubMed ]
6. Auerbach AD, Murff HJ, Islam SD. Pre-anesthesia checklists to improve patient safety. In: Shojania KG, Duncan BW, McDonald KM, Wachter RM, eds. Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment No. 43, AHRQ Publication No. 01-E058; July 2001. [ full report available ]
7. Smulian JC, Vintzileos AM, Rodis JF, Campbell WA. Community-based obstetrical ultrasound reports: documentation of compliance with suggested minimum standards. J Clin Ultrasound. 1996;24:123-7.[ go to PubMed ]
Figures
Figure 1. Bicornuate Uterus (cross section). The normal uterus has a single cavity without horns. (Inset. Bicornuate uterus.) (Illustration by Chris Gralapp)
Figure 2. Transvaginal view of uterus. Gravid bicornuate uterus, pregnancy in right horn (RH).