Dropping to New Lows
Case Objectives
- State how to manage diabetes medications when patients are admitted to the hospital
- Describe a guideline-recommended insulin regimen for a hospitalized patient
- Outline goal blood glucoses for patients with diabetes admitted to critical care and noncritical care settings
- Appreciate the importance of a multidisciplinary diabetes steering committee in guiding glycemic management
- Describe optimal organizational strategies that can improve inpatient glycemic control
- Describe electronic health record–based strategies to achieve optimal inpatient glycemic control
Case & Commentary—Part 1:
A 62-year-old man with type 1 diabetes was admitted to the hospital with osteomyelitis of the right foot and acute kidney injury. The patient had previously had a stroke. At baseline he had some cognitive deficits and received his nutrition through a percutaneous gastrostomy (feeding) tube. He also received small amounts of soft food by mouth. For his diabetes, at home he was on a complex regimen of twice daily insulin glargine (Lantus, a long-acting insulin), insulin NPH (another long-acting insulin) once in the morning, and regular (short-acting) insulin multiple times a day.
The patient's blood sugars were difficult to control during the first 3 days of his hospitalization. He had multiple episodes of critical hypoglycemia (blood sugars less than 50 mg/dL) as well as serious hyperglycemia (blood sugars > 300 mg/dL). The hospitalist caring for the patient consulted an endocrinologist to help with the glucose management.
Although previous WebM&M commentaries have addressed best practices in inpatient management of diabetes, new evidence and guidelines have emerged in the past decade. This case provides an opportunity for an update to describe optimal management of inpatient diabetes, especially in the era of the electronic health record.
Diabetes is prevalent in the inpatient setting and is an independent risk factor for poor clinical outcomes.(1-3) Hospital goals for the patient with diabetes are to (i) prevent hyperglycemia and hypoglycemia, both of which are associated with adverse outcomes (including death), (ii) minimize the length of the hospital stay, and (iii) ensure an effective and safe transition out of the hospital. Current guidelines for pharmacologic management of inpatient diabetes support the discontinuation of oral diabetes agents and other non-insulin therapies in most circumstances. Patients often have contraindications to their use while hospitalized, including NPO status (taking nothing by mouth), variable oral intake, acute renal failure, and receipt of IV contrast.(3)
In most instances, insulin is the preferred treatment during hospitalization as it allows easier titration to adjust to the ever-changing variables in the inpatient setting. The sole use of sliding scale insulin in the inpatient setting is strongly discouraged. The preferred route depends on the site of care: continuous intravenous insulin infusion has been shown to be the best method for achieving glycemic targets in the critical care setting, while scheduled subcutaneous insulin with a basal, nutritional, and correction regimen is recommended in the noncritical care setting.(3-5) Although this patient presented to the hospital with a complex home regimen of two long-acting insulins (glargine and NPH) and one short-acting insulin (regular), the preferred subcutaneous insulin regimen for inpatient glycemic management includes one long-acting and one short-acting insulin along with a correctional scale that uses the same short-acting insulin to cover for nutrition.(6) The choice of which short-acting insulin to use is made based on the frequency and form of nutrition ordered; a complete discussion of this is beyond the scope of this commentary.
Glycemic targets in the inpatient setting have evolved over the last 2 decades, moving from "tight" control to a more moderate target. The initial target of 80–110 mg/dL was based on a significant reduction in intensive care unit mortality in critically ill surgical patients treated with IV insulin targeted at normalizing blood glucose.(7) However, subsequent trials had mixed results and a meta-analysis of more than 26 studies, including the largest, NICE-SUGAR, showed increased rates of severe hypoglycemia and mortality in tightly (versus moderately) controlled cohorts.(8) This evidence established new standards and the current American Association of Clinical Endocrinologists and American Diabetes Association inpatient glycemic control guidelines were revised to initiate insulin therapy for persistent hyperglycemia greater than 180 mg/dL and to keep target glucose in the controlled, rather than tight, range.(3) Specifically, once insulin therapy is initiated, a glucose target of 140–180 mg/dL is recommended for most critically ill patients. Greater benefit may be realized at the lower end of this range and lower targets may be appropriate in select patients, but targets less than 110 mg/dL are no longer recommended.
For noncritically ill patients, targets are based on clinical experience and judgment, but premeal glucose less than 140 mg/dL and random glucose less than 180 mg/dL are generally recommended. Higher glucose ranges may be appropriate for terminally ill patients and those with severe comorbidities, while lower ranges may be appropriate for patients who tolerate tight glycemic control as outpatients.(3,6) Clinical judgment combined with ongoing assessment of the patient's clinical status, including changes in glycemic trends, illness severity, nutritional status, or concomitant medications that might affect glucose, should be incorporated into the daily decisions regarding insulin doses.(3) In the above case, given the patient's comorbidities, including his cognitive deficit and acute kidney injury as well as his continuous nutrition, his glucose target should probably be 140–180 mg/dL. This target could likely be achieved using a long-acting insulin (such as glargine or levemir) for basal coverage, a short-acting insulin (such as regular insulin every 6 hours) to cover for continuous tube feeds and a correctional scale using the same short-acting insulin.
Case & Commentary—Part 2:
The endocrinologist believed there were multiple reasons for the hard-to-control blood sugars including an active infection, acute kidney injury, variable oral intake, and tube feeds that were intermittently held. She also recognized multiple problems with the system that were contributing. The nurses caring for the patient would often "hold" the morning or evening doses of insulin if his blood sugars were found to be less than 200 mg/dL. Because these "holds" were not clearly charted in the electronic health record (EHR), providers were unaware of how much insulin had actually been given.
In addition, the widely fluctuating sugars were often not immediately entered into the EHR but would only appear at the end of the shift—when the glucometer that was used to measure the blood sugars was "docked" to the EHR and the blood sugar results uploaded into the system. Because of this, the providers were often reacting to old or incomplete data.
To solve the problem in the short term, a paper tracking system of insulin dosing, blood sugars, and vital signs was developed for the patient. These logs were kept in the (now nearly empty) paper chart and then uploaded into the progress notes in the EHR. The hospital information technology team, aided by a multidisciplinary task force that was convened to improve on the overall process and workflow for inpatient diabetes management, began working on modifying the EHR to integrate these improvements.
Building a hospital program to optimally manage inpatient blood glucoses is a complex task, involving multiple levels of management, including physicians, nursing staff, diabetes educators, care coordinators, dieticians, and informatics teams. As evidenced by this case, when communication between the nursing staff and the provider is suboptimal, it becomes difficult to figure out if and when insulin was administered and when insulin doses should be held. One organizational strategy that has been critical for effective programs is establishment of an interdisciplinary steering committee that meets regularly to implement best practices and address issues in a collaborative and timely manner.(9) This committee should include representatives from several disciplines that have stake in improving hospital-wide glycemic control. These groups typically involve participants from pharmacy, nursing, IT, physician groups (including hospitalists, intensivists, surgeons, endocrinologists, and other hospital physicians), as well as diabetes educators, quality and patient safety improvement staff, lab, dietary and nutrition services, and hospital administration. Order sets and hard-wired systems of care that support safe glycemic control are also essential in building a hospital program. Many hospital systems take it a step further and create a frontline glycemic management team to accelerate and reinforce practice guidelines as well as target individual patients or population of patients, and providers, in a more direct way.(10) One team structure that has been effective in our experience is having an inpatient diabetes team consisting of advanced practice nurses/clinical diabetes educators supervised by an endocrinology faculty member. The inpatient diabetes team can act as consultants, change agents, and educators. Consults are triggered by traditional calls or pages from the primary team as well as by proactive surveillance of glycemic outliers prompting pages to the primary team with recommended changes.(11)
Provider education is also an essential element in achieving glycemic control in the hospital. One mechanism to ensure education of all ordering providers is to require successful completion of a competency exam. The exam could be combined with a live lecture or built as an online module focusing on main inpatient glycemic concepts in a case-based format. Education in real time can be targeted toward specific providers. Outreach to an individual can be triggered by an event (e.g., a reported adverse event related to glucose management), by pharmacy during the order validation process (e.g., a pharmacist notices an unusual order), or even screening by a glucose management team using proactive surveillance of glycemic outliers (e.g., a glucose management team receives a daily report of all patients with a recorded blood sugar less than 70 mg/dL or > 180 mg/dL and can choose to reach out to specific providers).(11) Another form of provider education that has been trialed is a Hyperglycemia Grand Rounds (HGR). The HGR is a continuing education initiative comprised of a four-module seminar series focused on best practices in inpatient diabetes management. Between 2006 and 2013, these seminars have been presented as Grand Rounds to more than 12,000 health care providers at over 300 institutions nationally. More than 2000 participating health care professionals self-reported that the program had improved learner knowledge, performance, and outcomes, and had motivated specific changes in clinical practice. The survey was also able to help identify barriers to implementing best practices; the three most common barriers to implementation were insufficient of coordination among hospital team members, lack of institutional protocols, and time limitations.(12)
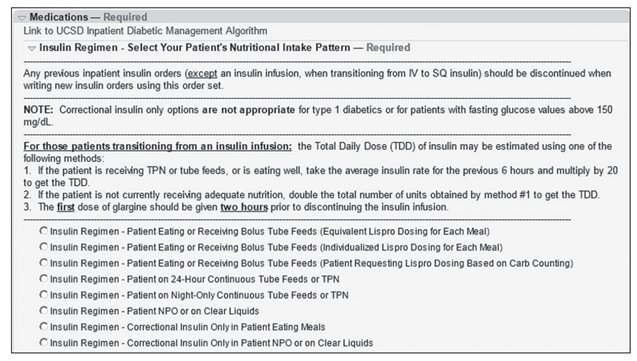
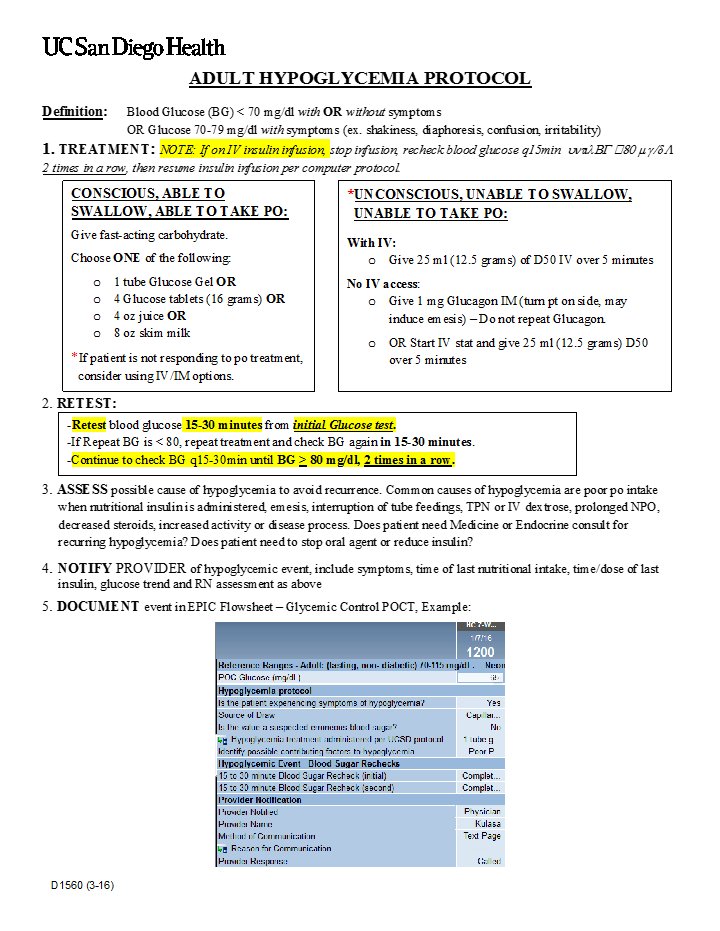
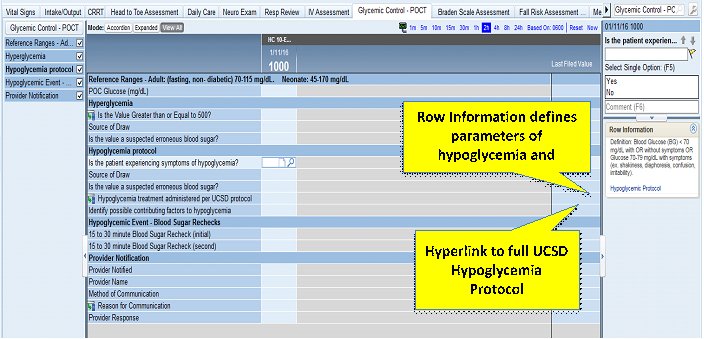
In addition to education, policies, algorithms, and protocols are crucial to building an inpatient diabetes management program. Protocol-driven and evidence-based order sets for specific clinical scenarios can help standardize insulin prescribing. Order sets can be designed for many scenarios, including transition from intravenous to subcutaneous administration, treatment of diabetic ketoacidosis, and treatment of hyperkalemia.(13) Order sets with built-in clinical decision support can help guide appropriate insulin ordering and glucose monitoring. An example of subcutaneous insulin orders in an electronic health record is seen in Figure 1. Here, insulin regimens are matched to various nutritional intake patterns; using order sets allows for incorporation of standardized administration instructions, indications, and holding parameters.(4,10-11) System-wide dissemination of these policies, algorithms, and protocols, as well as direct links throughout the electronic health record, can allow all providers and nursing staff to have immediate access to glucose management guidelines whenever questions should arise. Figures 2a and 2b show an example of a nurse-driven hypoglycemia protocol and a screenshot with direct links to the protocol from the electronic health record for easy access and reference. Once the protocols and order sets are disseminated, their use must be monitored and the process redesigned or protocols or order sets adjusted to ensure reliable use.(10)
In this case, the patient's tube feeds were intermittently held and nurses were often "holding" morning or evening doses of insulin if patient's blood glucose was less than 200 mg/dL. A previous WebM&M commentary specifically addressed how to optimally manage holding orders in the hospital, concluding that holding orders should be avoided unless absolutely necessary and that hold orders should provide specific instructions on when to resume the medication. In addition, the commentary described building a mechanism (presumably electronically) where the prescribing provider would be clearly notified when a medication has been held. In the present case, an ideal system would have automatically and clearly notified the provider when the insulin had not been given.
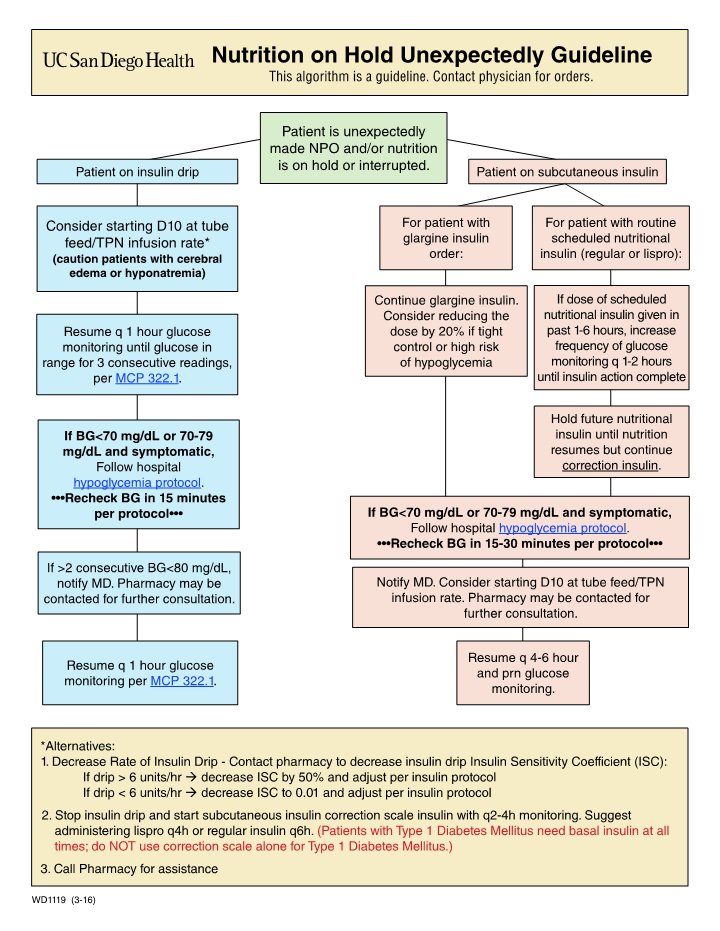
In addition to medications frequently being "held" in the hospital, food or nutritional intake is often temporarily stopped. If a patient is receiving insulin to match an expected caloric intake, stopping nutrition or tube feeding can lead to life-threatening hypoglycemia. Some institutions have standard algorithms to guide assessment and interventions when nutrition is unexpectedly held for a patient. Figure 3 shows one such guideline. Such algorithms are made even more useful when hyperlinks are added at appropriate places in the electronic medical record to allow for quick reference look up.(11)
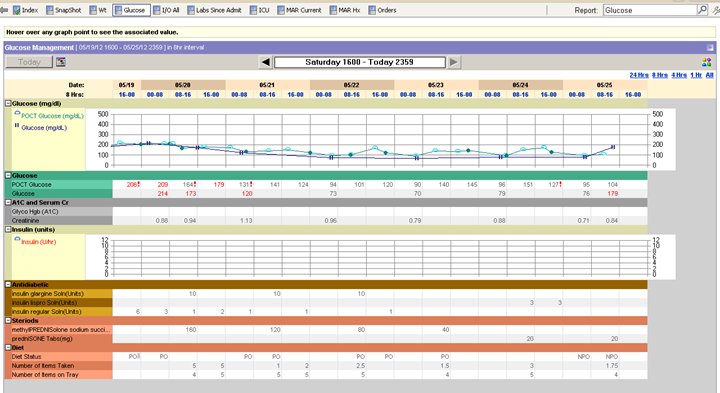
Electronic health records are particularly helpful in achieving optimal glycemic control, but only if information is quickly and easily accessible to providers. For example, a glucose management page that displays all necessary variables that impact glycemic control enables providers to quickly review glycemic trends and look for contributing factors such as insulin doses given, renal function, steroid dosing, and nutrition intake (Figure 4).
In the case above, the widely fluctuating sugars coupled with unclear documentation over whether insulin doses were actually given resulted in a complicated clinical scenario that was difficult for providers to disentangle. To facilitate inpatient glycemic management, glucometer readings need to be transferred to the electronic health record in real time, and insulin administration times and doses need to be clearly charted in a timely manner. Having easily accessible and timely glucose and insulin data is the only way providers can make appropriate adjustments to inpatient insulin regimens to prevent recurrent hypoglycemia and severe hyperglycemia. A multidisciplinary team approach to safe glycemic management is needed to build an inpatient glycemic program that is functional and effective.
Take-Home Points
- Target blood glucose for a critically ill patient is 140–180 mg/dL and an insulin infusion should be started for glucose greater than or equal to 180 mg/dL. General targets for the non-critically ill patient are premeal glucose less than 140 mg/dL and random glucose less than 180 mg/dL.
- "Tight" or euglycemic glucose control has been shown to increase mortality among critically ill patients.
- An interdisciplinary glycemic control steering committee that meets regularly (i.e., monthly) has been an essential element for successful programs.
- Electronic health records need to make glucose management information quickly and easily accessible to providers in order to be useful.
- Having extensive clinical decision support built into the electronic health record order sets is a way to quickly guide providers in ordering appropriate insulin regimens.
Patricia Juang, MD Assistant Clinical Professor of Medicine Division of Endocrinology, Diabetes, and Metabolism University of California, San Diego La Jolla, CA
Kristen Kulasa, MD Assistant Clinical Professor of Medicine Director, Inpatient Glycemic Control Division of Endocrinology, Diabetes, and Metabolism University of California, San Diego La Jolla, CA
Faculty Disclosure: Dr. Juang and Dr. Kulasa have declared that neither they, nor any immediate member of their families, have a financial arrangement or other relationship with the manufacturers of any commercial products discussed in this continuing medical education activity. In addition, the commentary does not include information regarding investigational or off-label use of pharmaceutical products or medical devices.
References
1. Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87:978-982. [go to PubMed]
2. Clement S, Braithwaite SS, Magee MF, et al; American Diabetes Association Diabetes in Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals. Diabetes Care. 2004;27:553-591. [go to PubMed]
3. Moghissi ES, Korytkowski MT, DiNardo M, et al; American Association of Clinical Endocrinologists and American Diabetes Association. American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Endocr Pract. 2009;15:353-369. [go to PubMed]
4. Maynard G, Wesorick DH, O'Malley C, Inzucchi SE; Society of Hospital Medicine Glycemic Control Task Force. Subcutaneous insulin order sets and protocols: effective design and implementation strategies. J Hosp Med. 2008;3(suppl 5):29-41. [go to PubMed]
5. Draznin B, Gilden J, Golden SH, et al; PRIDE Investigators. Pathways to quality inpatient management of hyperglycemia and diabetes: a call to action. Diabetes Care. 2013;36:1807-1814. [go to PubMed]
6. Umpierrez GE, Hellman R, Korytkowski MT, et al; Endocrine Society. Management of hyperglycemia in hospitalized patients in non-critical care setting: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2012;97:16-38. [go to PubMed]
7. van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359-1367. [go to PubMed]
8. Finfer S, Chittock DR, Su SY, et al; NICE-SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283-1297. [go to PubMed]
9. O'Malley CW, Ramos P, MacIndoe J, Manjarrez E, Maynard G, Nolan A. Characteristics of inpatient glycemic control among top performing hospitals [abstract]. J Hosp Med. 2015;10(suppl2). [Available at]
10. Glycemic Control Implementation Toolkit. Philadelphia, PA: Society of Hospital Medicine; 2015. [Available at]
11. Maynard G, Kulasa K, Ramos P, et al. Impact of a hypoglycemia reduction bundle and a systems approach to inpatient glycemic management. Endocr Pract. 2015;21:355-367. [go to PubMed]
12. Moghissi ES, Inzucchi SE, Mann KV, et al. Hyperglycemia grand rounds: descriptive findings of outcomes from a continuing education intervention to improve glycemic control and prevent hypoglycemia in the hospital setting. Hosp Pract (1995). 2015;43:270-276. [go to PubMed]
13. Cobaugh DJ, Maynard G, Cooper L, et al. Enhancing insulin-use safety in hospitals: practical recommendations from an ASHP Foundation expert consensus panel. Am J Health Syst Pharm. 2013;70:1404-1413. [go to PubMed]
Figures
Figure 1. Screenshot of Subcutaneous Insulin Orders in Electronic Health RecordFigure 2a. Example of Nurse-driven Hypoglycemia Protocol
Figure 2b. Example of Electronic Health Record Hypoglycemia Documentation
Figure 3. Algorithm to Guide Assessment and Interventions When Nutrition Is Unexpectedly on Hold
Figure 4. Screenshot of Glucose Management Page in Electronic Health Record