Are We Pushing Graduate Nurses Too Fast?
Spector ND. Are We Pushing Graduate Nurses Too Fast? . PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2011.
Spector ND. Are We Pushing Graduate Nurses Too Fast? . PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2011.
The Case
A middle-aged man was admitted to the surgical intensive care unit (SICU) following a complex surgical procedure performed for pancreatic cancer. He was on a ventilator, and several attempts to wean had been unsuccessful. The patient was also in acute renal failure. His current treatment included vasoactive drugs, intravenous fluids and nutrients, sedation, continuous renal replacement therapy (CRRT), and mechanical ventilation.
The registered nurse (RN) caring for this patient had completed nursing school 1 year earlier and had worked in this SICU since graduation; she had completed the hospital-based CRRT training in the prior month. In this hospital, RNs who regularly cared for SICU patients administered CRRT along with other care needed by the patient. RNs received special training in this technique from expert nurses in this hospital and received a certificate from the hospital after demonstrating their knowledge and skill.
The CRRT machine is supposed to have a bag of dialysate (solution with the appropriate chemicals and nutrients) infusing, and an ultrafiltrate bag connected to an outflow line, collecting the fluid being removed from the patient. During a conversation between two more senior nurses in the central nursing station, one glanced at the CRRT machine and noticed no dialysate bags; instead, there were two sets of ultrafiltrate bags. One set, full to capacity, was appropriately hooked into the ultrafiltrate line; the other empty set was hooked to the dialysate line. The senior nurse immediately stopped the CRRT machine and questioned the new graduate nurse caring for the patient. The newly trained nurse stated that there were no more bags of dialysate on the unit and she was trying to maintain the machine until some new bags arrived.
Before the new bags arrived and the CRRT could be restarted, the patient deteriorated and was taken back to surgery. He expired not long after from a perforated bowel.
Although the nurse's error in setting up the CRRT machine was not the direct cause of the patient's death, it did raise many questions. CRRT is a high-risk procedure that is handled differently by different hospitals. In some, only specially trained dialysis nurses administer this treatment; in others; the nurses on the units receive in-service training and manage the CRRT themselves. Questions that confronted the staff and critical care director for this unit were how to restructure the orientation and training programs to ensure that staff performing high-risk procedures were sufficiently prepared to anticipate problems, plan ahead, troubleshoot, and safely carry out the therapy.
The Commentary
Nursing is different from other health care professions in that there are several entry levels for the newly licensed RN (associate degree, diploma, baccalaureate, and master's degrees), thus making education more heterogeneous than for other caregivers such as physicians.(1) Although two recent national reports have called on RNs to all be educated to at least the baccalaureate level (2,3), this heterogeneity is likely to persist for the foreseeable future.
Every educational program for nurses must be approved by a State Board of Nursing, after showing they meet minimal standards. National accreditation of nursing programs, which requires a higher level of quality than state nursing board approval, is voluntary.(4) Before a license is granted, graduates of a nursing program must pass the national licensure examination that assesses minimal competency for entry to practice. Nursing programs are required to provide education and experiential learning in acute and chronic care. Although this education includes exposure to new technologies and administering complex clinical treatments at the unit level, it would be unrealistic to expect new graduates to have experience with every kind of therapy. Part of the problem is simply a matter of volume: on top of the traditional clinical nursing skills, new graduates face a daunting list of additional skills that they are expected to master, including being self-aware, understanding team dynamics, coordinating care, managing conflict, communicating across health care professionals, practicing quality improvement, employing evidence-based practice, and utilizing systems thinking in an environment of complexity and financial pressures.(5)
This case highlights a specific, more serious problem in nursing, one that adversely affects patients: How do newly licensed RNs transition from an educational environment to practice to assure safe patient care?
Currently, nursing does not require a standardized transition to practice program after graduation. There are no requirements for residencies or internships that provide guided experiences in applying the newly acquired knowledge. Therefore, this case is not an anomaly—instead it is commonplace in nursing. In other health care professions, such as medicine, pharmacy, pastoral care, and physical therapy, standardized residency programs are available and are the norm. Additionally, in 30 states, public school teachers are required to go through a mentorship induction program for 2 years following graduation, a program that is paid for by 17 states.(6)
Nurses' transitions from education to practice depend on what their employers offer them. This is quite variable and differs across educational levels of nurses.(7) A survey by the National Council of State Boards of Nursing (7), completed by 626 newly licensed RNs across practice settings and levels of education, shockingly found that 3% of the newly licensed RNs not only had no organized transition to practice program but also no orientation to the unit or institution. In the hospital setting, this study found that only 41% of the RNs reported having a comprehensive transition program that incorporated working with an experienced nurse (preceptorship), coupled with an orientation to the unit and a formal transition to practice program. In long-term care, only 22% of new RN graduates had a comprehensive transition program. Other studies confirm this variability in transition programs across settings and level of education in nursing.(8)
In part because of the paucity of postgraduate training, Benner (9) describes graduates in the first year of practice as being "advanced beginners." They have a heightened awareness of their need for continued learning and therefore benefit from continuous feedback from their colleagues and the health care team. They are anxious and report considerable fatigue, so coaching should incorporate strategies to ameliorate stress. Researchers have found a link between stress in new nurses and making errors.(10) Novice nurses, without a lot of experiential learning, don't have the ability to pick up subtle changes; they engage in concrete thinking and focus on technology and skills (9,11), thereby missing the bigger picture. This can adversely affect patient outcomes.(12) For example, Del Bueno (13) found that 50% of novice nurses miss signs of life-threatening conditions. Others (14) have found that inexperienced nurses sometimes omit key aspects of nursing care, which could lead to adverse outcomes.
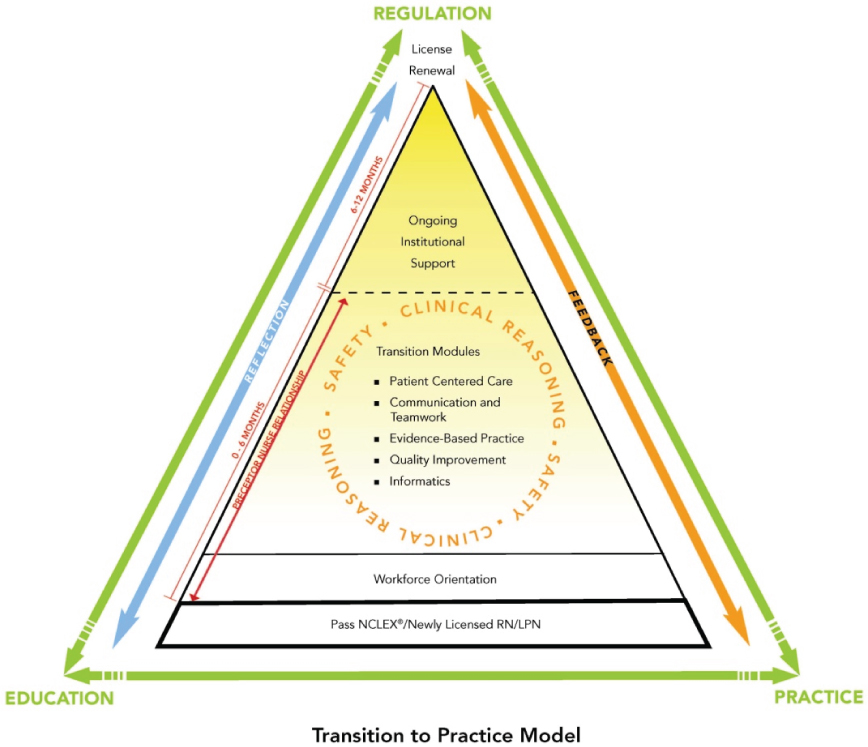
What should a comprehensive transition to practice program for nurses incorporate so that situations like this don't happen? The National Council of State Boards of Nursing developed an evidence-based model to transition new nurses to practice.(15) This was collaboratively built with leaders in regulation, education, and practice (Figure). Relevant to this case, in the patient-centered care module the institution is required to provide information on, and practice in, specialty content on the unit where the nurse would be working. For example, institutions might present simulations of critical events that that new nurses don't commonly see but that can be fatal to the patients. In this case, the new nurse in ICU might be presented with a simulation of the use of CCRT, which are high-risk procedures that new nurses would not commonly see. However, whatever the teaching strategy, the new nurses would be expected to have supervision until they have mastered the skill, as measured through a competency checklist or the evaluation of their preceptor.
A multi-site randomized study of this model, conducted in 150 sites across the United States, began in 2010 and data will be collected on actual patient outcomes and reports of errors and adverse events over several years. When the results of this study are analyzed, states will decide whether or not to require this model for all new nurse graduates. Perhaps a standardized transition program like this could have prevented the error that occurred in this case.
Take-Home Points
This case illustrates the following key points:
- Currently there are no requirements for transition to practice programs in nursing.
- Inadequate transition programs for newly licensed nurses can be related to adverse events, such as occurred in this situation.
- All newly licensed nurses should go through a standardized transition program that incorporates specialty content but also integrates concepts of patient-centered care, quality improvement, communication and teamwork, evidence-based practice and informatics, with clinical reasoning and safety integrated throughout. Providing feedback and opportunities for reflection should also be included.
Nancy Spector, PhD, RN Director of Regulatory Innovations, National Council of State Boards of Nursing Specializing in Nursing Education
References
1. Garman AN, Leach DC, Spector N. Worldviews in collision: conflict and collaboration across professional lines. J Organiz Behav. 2006;27:829-849. [Available at]
2. Benner P, Sutphen M, Leonard V, Day L. Educating Nurses: A Call for Radical Transformation. San Francisco, CA: Jossey-Bass; 2009. ISBN: 9780470457962.
3. Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health. Washington, DC: The National Academies Press; 2011. ISBN: 9780309158190. [Available at]
4. Spector N. Approval: National Council of State Boards of Nursing (NCSBN). In: Caputi L (ed). Teaching Nursing: The Art and Science. Vol 3. 2nd ed. Glen Ellyn, IL: College of DuPage Press; 2009. ISBN: 9781932514018.
5. Keller JL, Meekins K, Summers B. Pearls and pitfalls of a new graduate academic residency program. J Nurs Adm. 2006;36:589-598. [go to PubMed]
6. American Association of State Colleges and Universities. Policy Matters: Teacher induction programs: trends and opportunities. 2006;3. [Available at]
7. Kenward K, Zhong EH. Transition to Practice: Newly Licensed Registered Nurse (RN) and Licensed/Vocational Nurse (LPN/VN) Activities. Report of Findings from the Practice and Professional Survey, Fall 2004. National Council of State Boards of Nursing: Chicago, IL; 2006.
8. Scott ES, Engelke MK, Swanson M. New graduate transitioning: necessary or nice? Appl Nurs Res. 2008;21:75-83. [go to PubMed]
9. Benner P. Using the Dreyfus model of skill acquisition to describe and interpret skill acquisition and clinical judgment in nursing practice and education. Bull Sci Technol Soc. 2004;24:188-199. [Available at]
10. Elfering A, Semmer NK, Grebner S. Work stress and patient safety: observer-rated work stressors as predictors of characteristics of safety-related events reported by young nurses. Ergonomics. 2006;49:457-469. [go to PubMed]
11. Ebright PR, Urden L, Patterson E, Chalko B. Themes surrounding novice nurse near-miss and adverse-event situations. J Nurs Adm. 2004;34:531-538. [go to PubMed]
12. Orsolini-Hain L, Malone RE. Examining the impending gap in clinical nursing expertise. Policy Polit Nurs Pract. 2007;8:158-169. [go to PubMed]
13. del Bueno D. A crisis in critical thinking. Nurs Educ Perspect. 2005;26:278-282. [go to PubMed]
14. Spector N, Echternacht M. A regulatory model for transitioning newly licensed nurses to practice. J Nurs Regul. 2010;1:18-25. [Available at]
15. Transition to Practice. National Council of State Boards of Nursing: Chicago, IL; 2011.
Figure
Figure. Transition to Practice Model.