The Wrong Blade: A Lack of Familiarity With Pediatric Emergency Equipment
Katznelson J. The Wrong Blade: A Lack of Familiarity With Pediatric Emergency Equipment. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2018.
Katznelson J. The Wrong Blade: A Lack of Familiarity With Pediatric Emergency Equipment. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2018.
The Case
As part of a prospective multicenter cohort study, 58 interprofessional teams—each comprised of 1–2 physicians, 3–5 nurses, and 2–3 nursing assistants or emergency medical technician personnel—were evaluated in their native pediatric or general emergency department (ED) resuscitation bays as they managed a series of 3 simulated critically ill patients (sepsis, seizure, and cardiac arrest). The simulated cardiac resuscitation case was a 5-year-old boy, found pulseless and apneic in the bathtub by a parent. All of the teams used the Broselow system, a proprietary system designed to facilitate finding the appropriate-sized resuscitation equipment for ill and injured children requiring lifesaving interventions.
In the simulation case reviews, it was noted that many of the teams had difficulty with the resuscitation because of a lack of interoperability between the prestocked disposable laryngoscope blades and handles on the Broselow cart with the ED's actual stock of blades and handles. This incompatibility led to significant delays in intubation; at times, it led to actual failure to intubate. For example, the teams, who usually did not recognize the problem with compatibility, spent unnecessary time replacing batteries and the like. Some called for backup airway teams, resulting in delays in treatment. If this case were to actually occur, it is likely that many of the teams would have made significant errors in handling the intubation equipment that would likely have led to patient harm or even death.
The Commentary
Commentary by Jessica Katznelson, MD
There are nearly 74 million children under the age of 18 in the United States.(1) One in five children seeks care in an emergency department (ED) each year; most receive their care in a community hospital setting.(2) Yet, on average, only 16% of emergency medicine residency training time is pediatric-focused.(3) Moreover, most EDs do not have pediatric emergency–trained physicians, nurses, or respiratory therapists on their staff, or a pediatrician on site. This leaves children to be cared for mainly by adult-trained staff who may be less comfortable with pediatric presentations and the age-appropriate equipment and resources needed to treat them.
Pediatric cardiopulmonary resuscitation is a fairly rare event in pediatric EDs in academic medical centers and even more rare in the community ED setting. There are limited patient data on the quality of pediatric resuscitation in either of these settings, but data suggest an "all comers" survival rate of approximately 8% for out-of-hospital arrests, with higher survival rates for those whose arrest occurs in a hospital setting.(4) In the case study described above, there were significant delays in intubation at some of the sites due to a lack of intraoperability between the pediatric-specific intubation equipment (Broselow) used for the scenario and the other intubation equipment stocked in the ED. This delay is concerning but unsurprising given the low frequency of such events and lack of training of ED personnel.
Simulation has become a widely used teaching tool in the academic medical center setting. Simulation allows teams to practice skills and teamwork and to utilize equipment that may be rarely used—all in a safe setting where no patient harm is possible. Simulation can improve team resuscitation performance and comfort with pediatric patients.(5,6) Moreover, simulation can assess for latent patient safety threats, particularly in the pediatric setting.(7,8) Hospitals with larger pediatric volumes perform better in simulated pediatric resuscitations.(5) However, even in children's hospitals, residents were found to not meet American Heart Association guidelines with regards to time to compressions and defibrillation.(9) Moreover, cognitive aids did not improve performance.(10) A PubMed literature search revealed few studies addressing the issue of correctly sized equipment for pediatric resuscitation. The studies that were done spoke to the benefits of a color-coded, weight-based system for equipment storage and medication dosing.
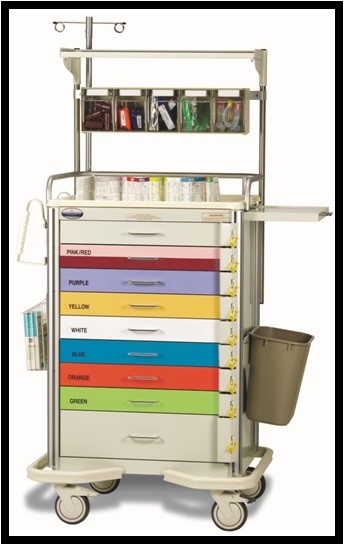
The Broselow cart (Figure) is a proprietary system that utilizes a color-coded cart. Each drawer is a different color, corresponds to a different weight range, and is stocked with appropriately sized resuscitation equipment for a patient of a given size. Moreover, the colors correlate to those on the Broselow tape—a tool that allows length-to-weight conversions and documents weight-based resuscitation equipment sizes and drug doses. Multiple studies suggest that equipment is found faster, fewer errors are made, and medications are more likely to be dosed correctly using such a system.(11,12)
The problem with the intubation equipment described in the scenario is due to the proprietary nature of the system. Broselow laryngoscope blades are designed to only fit on Broselow laryngoscope handles, which becomes a potential safety issue in community EDs that stock both Broselow and non-Broselow equipment. A care provider may inadvertently try to use a Broselow blade with a non-Broselow handle or vice versa. As the simulated cases show, this has the potential to lead to significant delays in intubation.
The American Academy of Pediatrics, along with the American College of Emergency Medicine, has compiled a list of the recommended pediatric equipment and specifies sizes for the equipment to be stocked in most EDs.(13) This list includes intubation and other resuscitation equipment of all sizes from neonate to adult. Today, most hospitals stock most, if not all, of the equipment on the list, and most community and many academic EDs have chosen to use the Broselow system. However, there are no mandates regarding what brand of equipment is used or that there be any interoperability between systems.
The simple solution to the laryngoscope blade and handle issue would be to ensure compatibility between different manufacturers' products. However, these systems are proprietary and that would be difficult, if not impossible, to mandate. Moreover, the issues extend beyond just intubation equipment. Emergency departments need to be able to rapidly access correctly sized pediatric equipment of all types (for example, endotracheal tubes, foley catheters, nasogastric tubes, etc.) and to be familiar with their use. In such situations, simulation can be especially helpful.
It makes sense to continue with the Broselow system in most EDs. There is good data that it is helpful (12), and a proven alternative that will reliably allow ED personnel to choose appropriate-sized equipment for children of various sizes has not been identified. Widespread adoption of simulation in the community hospital ED setting would allow teams to become adept at rapidly accessing and comfortable using pediatric resuscitation equipment, all in a no-risk setting that would enable the identification of latent patient safety threats before they harm a child. Pediatric resuscitation is always going to be a low-frequency event. Simulation can allow medical teams to become confident and competent to care safely for these high-risk patients.
Take-Home Points
- Most children seen in the emergency department are cared for by nonpediatric emergency–trained physicians.
- Emergency medicine physicians receive limited pediatrics training.
- There are fewer medication and equipment errors when the Broselow system is used, but issues of compatibility between this system and existing emergency department equipment can threaten patient safety.
- Simulation can help identify latent patient safety threats and can be used to increase pediatric preparedness in emergency departments.
Jessica Katznelson, MD
Assistant Professor of Pediatrics and Emergency Medicine
Johns Hopkins School of Medicine
References
1. Child Health USA 2014. Rockville, MD: U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau; 2014. [Available at]
2. Gauche-Hill M, Schmitz C, Lewis RJ. Pediatric preparedness of US emergency departments: a 2003 survey. Pediatrics. 2007;120:1229-1237. [go to PubMed]
3. Cloutier RL, Walthall JDH, Mull CC, Nypaver MM, Baren JM. Best educational practices in pediatric emergency medicine during emergency medicine residency training: guiding principles and expert recommendations. Acad Emerg Medicine. 2010;17(suppl 2):S104-S113. [go to PubMed]
4. Jayaram N, McNally B, Tang F, Chan PS. Survival after out-of-hospital cardiac arrest in children. J Am Heart Assoc. 2015;4:e002122. [go to PubMed]
5. Auerbach M, Whitfill T, Gawel M, et al. Differences in the quality of pediatric resuscitative care across a spectrum of emergency departments. JAMA Pediatr. 2016;170:987-994. [go to PubMed]
6. Katznelson JH, Wang J, Stevens MW, Mills WA. Improving pediatric preparedness in critical access hospital emergency departments: impact of a longitudinal in situ simulation program. Pediatr Emerg Care. 2018;34:17-20. [go to PubMed]
7. Patterson MD, Geis GL, Falcone RA, LeMaster T, Wears RL. In situ simulation: detection of safety threats and teamwork training in a high risk emergency department. BMJ Qual Safety. 2013;22:468-477. [go to PubMed]
8. Wetzel EA, Lang TR, Pendergrass TL, Taylor RG, Geis GL. Identification of latent safety threats using high-fidelity simulation-based training with multidisciplinary neonatology teams. Jt Comm J Qual Patient Saf. 2013;39:268-273. [go to PubMed]
9. Hunt EA, Vera K, Diener-West M, et al. Delays and errors in cardiopulmonary resuscitation and defibrillation by pediatric residents during simulated cardiopulmonary arrests. Resuscitation. 2009;80:819-825. [go to PubMed]
10. Nelson McMillan K, Rosen MA, Shilkofski NA, Bradshaw JH, Saliski M, Hunt EA. Cognitive aids do not prompt initiation of cardiopulmonary resuscitation in simulated pediatric cardiopulmonary arrests. Simul Healthc. 2018;13:41-46. [go to PubMed]
11. Maul E, Latham B, Westgate PM. Saving time under pressure: effectiveness of standardizing pediatric resuscitation carts. Hosp Pediatr. 2016;6:67-72. [go to PubMed]
12. Agarwal S, Swanson S, Murphy A, Yaeger K, Sharek P, Halamek LP. Comparing the utility of a standard pediatric resuscitation cart with a pediatric resuscitation cart based on the Broselow tape: a randomized, controlled, crossover trial involving simulated resuscitation scenarios. Pediatrics. 2005;116:e326-e333. [go to PubMed]
13. American Academy of Pediatrics; Committee on Pediatric Emergency Medicine; American College of Emergency Physicians; Pediatric Committee; Emergency Nurses Association Pediatric Committee. Joint policy statement—guidelines for care of children in the emergency department. Pediatrics. 2009;124:1233-1243. [go to PubMed]
Figure
Figure. Broselow Cart.