Volume Too Low: In and Out
Case Objectives
- Appreciate that because of multiple factors, children are at high risk for medical errors.
- Describe the importance of weight-based dosing of medications and fluids in pediatrics.
- Describe how the inability to communicate clearly can place pediatric patients at risk for medical errors or unsafe care.
- List two interventions that may help providers more safely care for pediatric patients.
The Case
A 22-month-old infant was admitted to the hospital in the late afternoon with a viral infection. He had a complex past medical history including congenital heart disease, poor feeding requiring a gastric tube, and delayed cognitive development. At the time of admission, he was moderately ill appearing but remained interactive with his mother and hospital staff. He was given appropriate therapies for his viral infection.
Later in the evening, the infant drank 2 ounces (60 mL) of a liquid nutritional drink and then went to sleep; this was the sum total of his fluid consumption since hospital admission. The child slept well and in the morning his vital signs were all normal. He remained interactive but seemed a bit sleepy. His total urine output overnight as documented by the nurse was 50 mL (a low urine output given his weight of 10 kg). The night nurse communicated the minimal intake of fluids and poor urine output to the day nurse at the 7:00 AM change of shift.
The day nurse, busy caring for other patients, failed to appreciate the significance of the low intake and output. Over the next few hours, the infant became more somnolent and less responsive. His aunt assumed this was due to the viral infection, and the child was not evaluated by the nurse during this time. When his mother returned in the early afternoon, she found her son to be lethargic and acting strangely. Evaluation by the intern revealed a low blood pressure, high heart rate, decreased muscle tone, and decreased responsiveness to stimulation. Stat labs revealed severe hypoglycemia and dehydration. The infant was transferred to the pediatric intensive care unit where an IV was placed and he was given intravenous fluids and intravenous glucose. He required 2 days in the intensive care unit but did not experience any long-term consequences.
The Commentary
This infant's case highlights two of the major risks that hospitalized children face from a patient safety perspective: the need to quantify therapies and assessments based on weight and the inability of children to communicate with health care providers (in this case, a patient who is unable to say, "I am really thirsty"). In addition, this case also reveals the specific risks of dehydration in patients with congenital heart disease.
Overall, the distinctive factors behind children's risks for patient safety events have been summarized in terms of development, demographics, dependency on parents and other care providers, and differential epidemiology.(1) Woods and colleagues detailed these pediatric patient safety risk factors as involving three key overarching domains: physical characteristics, developmental issues, and minor legal status issues.(2) For example, the recommended energy intake, normal blood pressure ranges, daily fluid intake requirements, and medication doses in pediatrics all vary with age and/or weight of the child. Those who care for children need to be aware of these varying ranges of 'normal' and adjust their management accordingly. There are also specific risks related to medication. Stages of development usually require liquid medication preparations at young ages as opposed to tablets. As some medications are not readily available in liquid suspensions, pharmacists may have to manually prepare suspensions by crushing tablets, which can lead to dosing errors. Young children also are completely dependent on caregivers for all aspects of medical care, including medication administration even in the ambulatory setting. These types of issues, which all predispose to patient safety events, are largely nonissues for adult patients. The net effect of these risks, however summarized, is that for some aspects of medical care, children are at substantially greater risk for medical errors and adverse events than adult patients.
The most easily understood high risk area for children is centered on the need to quantify therapies and assessments relative to weight (one of the main errors in this case). A simple example can best illustrate this risk. Imagine you and four adult colleagues sitting together in a room all simultaneously suffer from a headache and all decide to take ibuprofen. As each of you pulls out your pills or 'dose,' four of you decide to each take between 200 mg and 800 mg. The fifth colleague puts 3,000 mg on the table. In the blink of an eye, the other four colleagues instantly know that dose is wrong. The proper dose for an adult is generally recognizable, so that computer tools or more sophisticated calculations are not needed. In sharp contrast, in the average children's hospital, the range of patients' body weight can vary from 250 grams (in the neonatal intensive care unit) to 250 pounds, or 114 kg, for a hefty adolescent. This is a 450-fold weight variation! No pediatric provider, physician, pharmacist, or nurse can rely on an intuitive sense or prior experience that a medication dose is 'too high' or an output (as in this case with the infant's urine output) is 'too low.' Instead, for nearly every aspect of pediatric care both in and out of the hospital, it is essential that therapies and issues such as fluid monitoring be assessed relative to weight.
An extensive body of literature describes medication errors related to weight-based dosing in pediatric patients. We know that errors in prescribing, dispensing, and administering medications represent a substantial portion of the preventable medical errors in children and that children are at many-fold greater risk than adults for medication errors.(3-6) Fluids, both administered to patients and tracked as outputs, also have clearly defined normal parameters that are weight dependent and fluctuate with age. For example, standard fluid requirements for children are 4 mL/kg body weight/hour for the first 10 kg of weight; 2 mL/kg body weight/hour for the second 10 kg of weight; and 1 mL/kg body weight/hour for each additional kilogram past 20.(7) Using this recommendation, typical fluid requirements for a 25 kg child would be 65 mL per hour (4 mL/kg/hour x 10 kg = 40 mL/hour for the first 10 kg; 2 mL/kg/hour x 10 kg = 20 mL/hour for the second 10 kg; 1 mL/kg/hour x 5 kg = 5 mL for the last 5 kg; 65 mL/hour for a 25 kg child). In the case discussed here, the patient's weight was 10 kg, which translates into a fluid requirement of 40 mL/hour or 960 mL/day (4 mL/kg/hour x 10 kg x 24 hours = 960 mL/day). The 2 ounces our case patient consumed on the first day of admission was only 60 mL, representing a 900 mL deficit! Comparably, acceptable urine output varies with both body weight and patient age. In infants, typically considered younger than 1 year of age, oliguria (abnormally low urine output) is defined as 7) In our case example, this infant had 50 mL output in approximately 12 hours which translates to 0.2 mL/kg body weight/hour, well below expected. Depending on the pediatric-specific training of providers, or lack thereof, the inputs and outputs may have seemed 'normal' since a 10 kg infant can appear so substantially smaller than an adult, but weight-based quantification reveals the significant inadequacy of both in the intake and output.
Challenges of communication due to developmental stage also exposed this patient, and potentially expose most children, to risk. Infants, children, and patients with developmental delay issues cannot be active partners in their own medical safety. This may manifest itself as simply as the inability to communicate complaints clearly (e.g., "I am thirsty" or "I have pain"). Moreover, pediatric patients may also be unable to ask questions or advocate for themselves. A 4-year-old will not ask why they are taking a new medicine, and an infant cannot make sure the physician is working under sterile conditions. Instead, children must rely on proxies such as parents and guardians. Even under the best of circumstances, parents/guardians may need to occasionally leave their hospitalized children, not only for personal care but also work or other life demands. When this occurs, these vulnerable populations must rely solely on medical staff for their protection from errors and adverse events. Knowing that no system or provider is perfect, children and those with developmental disabilities are inherently at heightened risk. In this case, had the patient been a cognitively intact adult or teen, he could have helped avoid this event by simple verbal communication of thirst.
This case also highlights some of the unique physiologic challenges in pediatric patients with congenital heart disease. Although this case does not specify the exact type of congenital heart disease nor whether it has been repaired, a substantial percentage of infants and children with both repaired and unrepaired congenital heart disease are unable to withstand even mild to moderate dehydration. Decreased myocardial function or ejection fraction, increased systemic vascular resistance, and persistence of systemic-to-pulmonary intravascular shunts can make even minor degrees of dehydration potentially fatal. Because of this, the underlying congenital heart disease should have triggered providers to be even more vigilant than usual about monitoring the fluid intake and urine output.
How could the errors in this case have been prevented? The easiest solution was likely as close by as a calculator. Ordering medications, fluids, and even tracking outputs in all infants and children should be quantitatively calculated and recorded using appropriate body weight–based algorithms. In cases in which providers are not intimately versed in pediatric fluid management, intuitive alarm bells may not sound at seeing 50 mL of urine output overnight, since an infant appears so much smaller than an adult. In this case, the institutional expectation and standard of care should have been assessment and reporting of all intakes and outputs as mL/kg of body weight/hour. One would hope that all providers involved in the care would be trained to recognize abnormal values and would note if the urine output were too low. A more elaborate but obvious solution lies in computerized ordering as well as computerized recording of daily inputs/outputs flow management. Commercial ordering and tracking tools can and must be customized to include pediatric parameters, coupled with alert parameters that trigger alarms for outlier results. The investments in both time and money to build this type of information technology will be far exceeded by the removal of mathematical errors and oversights in calculating all pediatric medications, fluids, and outputs.
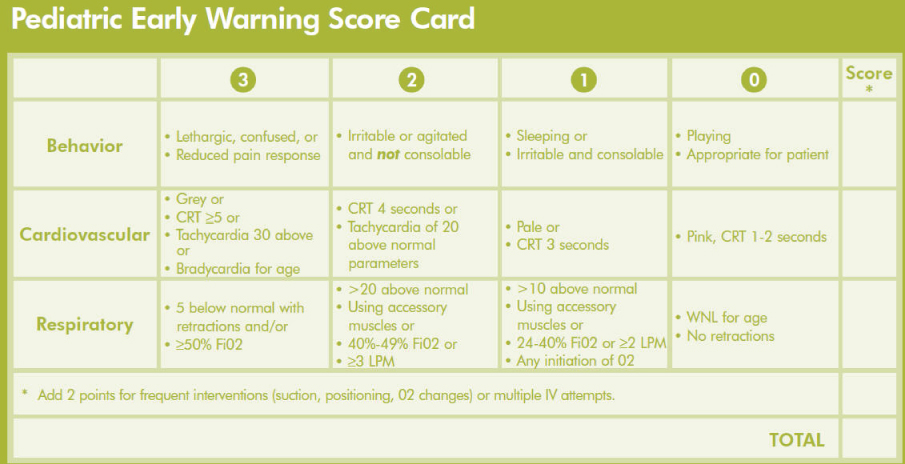
This event could also have potentially been mitigated with the interventions of pediatric early warning scores or rapid response teams. In pediatric early warning scoring (PEWS), aspects of behavior, cardiovascular status, and respiratory status are routinely monitored and tracked to identify clinical declines earlier. The Figure shows an example of a pediatric early warning score card; a child is felt to be at risk if there are ≥ 4 points total or ≥ 3 points in any of the three main domains (behavior, cardiovascular, respiratory). There is good evidence supporting their use; one recent study of PEWS reported a >11-hour forewarning of clinical declines (8), while another showed that PEWS could have identified 87% of hospitalized children who were "at risk" for deterioration.(9) Alternatively, had a pediatric rapid response team been in place, the standard resuscitative algorithm of Airway, Breathing, Circulation would likely have identified decreased peripheral perfusion due to dehydration and could have averted the need for intensive care via sooner fluid bolus administration.(10,11)
In summary, this case illustrates many of the unique aspects of care of children that predispose pediatric patients to patient safety events. The standard of care for children clearly involves a keen awareness of the importance of age/weight based considerations in all aspects of pediatric care. All providers of care to children should be aware of these considerations and aided in implementing and adhering to them.
Take-Home Points
- Many aspects of the care of children require age and/or weight-based considerations to understand what is 'normal' for children. These aspects include almost all medication dosing, nutrition management, fluid intake, fluid outputs, and even equipment sizes.
- Providers of care for children need to be well versed in these age/weight considerations.
- Tools to assist in managing children, such as computerized bedside management systems (that can both create orders as well as track fluids and output) and early warning score cards, can aid in the appropriate and safe care of children.
Marlene Miller, MD, MSc Vice Chair, Quality and Safety
Johns Hopkins Children's Center
Baltimore, MD
Faculty Disclosure: Dr. Miller has declared that neither she, nor any immediate member of her family, has a financial arrangement or other relationship with the manufacturers of any commercial products discussed in this continuing medical education activity. In addition, the commentary does not include information regarding investigational or off-label use of pharmaceutical products or medical devices.
References
1. Santell JP, Hicks R. Medication errors involving pediatric patients. Jt Comm J Qual Patient Saf. 2005;31:348-353. [go to PubMed]
2. Woods DM, Holl JL, Shonkoff JP, Mehra M, Ogata ES, Weiss KB. Child-specific risk factors and patient safety. J Patient Saf. 2005;1:17-22. [Available at]
3. Miller MR, Robinson KA, Lubomski LH, Rinke ML, Pronovost PJ. Medication errors in paediatric care: a systematic review of epidemiology and an evaluation of evidence supporting reduction strategy recommendations. Qual Saf Health Care. 2007;16:116-126. [go to PubMed]
4. Kaushal R, Jaggi T, Walsh K, Fortescue EB, Bates DW. Pediatric medication errors: what do we know? What gaps remain? Ambul Pediatr. 2004;4:73-81. [go to PubMed]
5. Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285:2114-2120. [go to PubMed]
6. McPhillips HA, Stille CJ, Smith D, et al. Potential medication dosing errors in outpatient pediatrics. J Pediatr. 2005;147:761-767. [go to PubMed]
7. Johns Hopkins Hospital, Custer JW, Rau RE, Lee CK. Harriet Lane Handbook, 18th Edition. St. Louis, MO: Mosby; 2008. ISBN: 9780323053037.
8. Akre M, Finkelstein M, Erickson M, Liu M, Vanderbilt L, Billman G. Sensitivity of the pediatric early warning score to identify patient deterioration. Pediatrics. 2010;125:e763-e769. [go to PubMed]
9. Tume L. The deterioration of children in ward areas in a specialist children's hospital. Nurs Crit Care. 2007;12:12-19. [go to PubMed]
10. Hunt EA, Zimmer KP, Rinke ML, et al. Transition from a traditional code team to a medical emergency team and categorization of cardiopulmonary arrests in a children's center. Arch Ped Adol Med. 2008;162:117-122. [go to PubMed]
11. Sharek PJ, Parast LM, Leong K, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU of a children's hospital. JAMA. 2007;298:2267-2274. [go to PubMed]
Figure
Figure. Sample Pediatric Early Warning Score Card. A child is felt to be at risk if score is ≥ 4 points total or ≥ 3 points in any of the three main domains (behavior, cardiovascular, respiratory).