Total Parenteral Nutrition, Multifarious Errors
Boullata JI. Total Parenteral Nutrition, Multifarious Errors. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2013.
Boullata JI. Total Parenteral Nutrition, Multifarious Errors. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2013.
Case Objectives
- Define parenteral nutrition (PN).
- Describe the PN-use process.
- Identify potential PN-related medication errors.
- Describe methods to reduce PN-related errors.
Case & Commentary—Part 1
A 3-year-old boy on chronic total parenteral nutrition (TPN) due to multiple intestinal resections was admitted to an academic medical center for anemia. At baseline, the boy was developmentally appropriate but quite fragile medically, with multiple recent admissions for anemia and infections. Unable to take anything by mouth, he was completely dependent on the TPN for his nutrition and fluid intake, and had been so for more than a year. The boy had been doing well at home when he began having small amounts of bloody output from his ostomy site. His mother (the patient's primary caretaker at home) brought him to the hospital and he was admitted for further evaluation of the anemia. At the time of admission he was continued on his home TPN regimen.
The patient described in this case was receiving parenteral nutrition (PN), a life-sustaining therapy for individuals who cannot maintain or improve their nutrition status through the oral/enteral route. Such therapy is used in patients of all ages and across care settings (from intensive care units to the home). More than 350,000 hospital stays per year include PN, and tens of thousands of patients continue PN use at home.(1) During growth and development, PN is particularly important for children even when the PN solution does not provide the total nutrient needs of a patient. Anticipated adverse effects of PN include complications associated with intravenous access (e.g., thrombosis, bloodstream infection) and metabolic homeostasis (e.g., hyper- or hypoglycemia, fluid and electrolyte disorders). The risks associated with PN were addressed at a recent safety summit.(2)
High-Alert Medication, Complicated Process
What may be less well recognized is that PN has been characterized as a high-alert medication.(3) High-alert medications, by definition, are those that involve risk for significant harm when used in error. As such, safeguards are required to minimize error risk from PN. Notably, a patient's daily PN admixture may contain at least 40 active ingredients, each with dosing implications and interaction potential.
Even though the ingredients in PN may carry some risk, errors in the PN-use process may lead to even more safety hazards. The PN-use process refers to the numerous steps in providing PN therapy, including prescribing, order review, preparation (compounding) and labeling, dispensing, administration, monitoring, as well as ongoing patient assessment and documentation of each step.(1) These steps also involve numerous clinicians and caregivers from several departments, if not more than one organization or facility. Without a standardized process and full collaboration, many opportunities for error arise.(4) Although errors are known to occur, a limited number of publications discuss them. Such errors may easily result in PN ranking among the top causes of medication error, but very few organizations capture these or share them internally.(5) Moreover, unlike other high-risk medications, such as insulin or anticoagulants, limited literature describes the errors associated with PN use. A lone prospective observational study at one institution identified 74 PN-related medication errors (16 per 1000 PN prescriptions), with most occurring during transcription (39%), preparation (24%), and administration (35%).(4) Because this group had a nutrition support team that wrote the prescriptions, no PN ordering errors were identified that resulted in an incorrect admixture or subsequent patient harm. This structure is optimal but atypical, and mistakes in the PN prescription and in the PN order review process may contribute to additional harm and a significant number of errors not captured in this study. Nearly 10% of the errors identified resulted in or contributed to patient harm.(6)
Making PN Use Safer
In addition to standardization of the process and the expertise of those involved, the number of patients receiving PN is a critical factor. Most institutions manage fewer than 10 PN patients daily, and more than 80% manage 5 or fewer pediatric patients requiring PN.(5) Although this number may reflect appropriate PN use in favor of enteral nutrition when indicated, it also reveals the limited experience with PN in many organizations. The expertise needed to safely manage patients requiring PN is analogous to the expertise expected in the drug-use process for cancer chemotherapy. Health care providers involved with PN should be knowledgeable and skilled in patient PN management and error prevention. Caregivers involved with PN should work within an interdisciplinary setting that includes certified nutrition support nurses, pharmacists, dietitians, and physicians.(7)
Despite being a complex and high-alert medication, only 58% of organizations have safeguards in place to prevent patient harm from errors in the PN-use process.(8) Approaches to improving the safety of PN can encounter significant organizational challenges but can be successful when based on published practice guidelines and standards.(9) To help organizations minimize errors when using use this complex therapy, practice guidelines and recommendations (based on evidence or generally accepted practices) are available from national organizations. The American Society for Parenteral & Enteral Nutrition (ASPEN) published the safe PN practice guidelines (10), but surveys have found that these guidelines have poor adherence.(5,11,12) Meaningful reductions in error rates have been reported in a pediatric setting that adopted a standardized PN process.(13) A revision of the 2004 ASPEN document is under way to provide graded, evidence-based clinical guidelines and a set of specific, actionable practice recommendations based on expert consensus.(5)
Transitions in Care and PN
Transitions in care create the opportunity for medication-related errors, which is certainly true for PN. One major contributing factor is the lack of prescription uniformity between institutions and across patient care settings; this variation is unmatched by any other medication in clinical practice. Myriad methods of ordering and labeling these complex PN preparations can be found. For example, varied units-of-measure can cause significant errors especially during transitions between hospital and home (14), at the least, errors involving the dosing of one or more of the dozens of active ingredients. Misinterpreted information from a PN label has led to error and patient harm in the transition from home to hospital.(10)
Ideally, one would hope the hospital described in the above scenario manages a high volume of patients on PN and adheres to the recognized national guidelines.(10) Their staff members should be well-trained in all steps of the PN-use process, and the hospital should have a standardized process to reduce the risk for errors.
Case & Commentary—Part 2
On hospital day 2, the patient's serum sodium was noted by the team to be low at 130 mEq/L (normal 135–145 mEq/L). The team ordered to increase the amount of sodium in the TPN from 5.2 mEq/kg/day to 5.5 mEq/kg/day based on a standard formula. The new TPN with the increased sodium began infusing at 9:00 PM. Overnight, the boy complained of worsening abdominal pain, which was treated with increased doses of intravenous opiates. He also complained of headache (which he never had previously, per the mother) and was irritable and could not be consoled. In the morning, his labs were notable for serum sodium of 158 mEq/L, which was confirmed on recheck. At first, the acute hypernatremia was attributed to dehydration. On rounds, the resident caring for the patient examined the TPN bag to see how much sodium the boy was receiving. The TPN bag had a sodium concentration of 55 mEq/kg/day (a 10-fold increase of the intended sodium concentration of 5.5 mEq/kg/day). The TPN was immediately stopped and the boy was given free water intravenously to correct the severe hypernatremia. Correction took more than 48 hours. Fortunately, the boy did not experience any adverse consequences from the hypernatremia.
On formal review of the case, multiple errors led to the excess sodium infusion. This academic medical center had a functioning electronic health record (EHR) and computerized provider order entry (CPOE) system. However, due to the complexity of TPN orders, they were completed by hand and then scanned to the pharmacy to be entered by the pharmacist into the CPOE system. The order for the increased sodium was written appropriately on the paper order, which was scanned to the pharmacy. The pharmacist (who was specifically trained to enter TPN orders) inadvertently entered 55 mEq/kg/day into the computer. A second pharmacist (also trained in TPN) reviewed the order by standard protocol and did not catch the dosing error. The order was then sent to the contracted pharmacy that prepared the TPN for this hospital, and there an additional two TPN pharmacists did not recognize the error. Automatic warning flags popped up in the system regarding the high sodium dose but these were ignored and dismissed as this boy had more than 8 warnings each day for his TPN order, even when entered correctly.
Speaking with the pharmacists revealed that there was not only an error in transcription but they also had incorrectly perceived 55 mEq/kg/day as 55 mEq/L/day, an appropriate dose for an adult TPN order. Because of this, the TPN order was produced with the high sodium concentration and sent to the hospital. Two nurses verified the TPN order was accurate and appropriate at the bedside and also did not notice the error.
The error in this case involved a breakdown in oversight and system checks; breakdowns leading to medication errors is a familiar scenario.(14) PN-related dysnatremia may be an all too common—though infrequently documented—error. As occurred in this case, multiple failures across the PN-use process are usually identified in retrospect as contributing to such errors. These can involve order entry and transcription errors, inappropriate abbreviations, dose designations or units-of-measure, PN component mix-ups (a bigger concern with ongoing shortages of many of these components), no warnings for catastrophic dose limits, catheter misconnections, and ineffective or nonexistent systems of independent double-checks.(14) However, as happened here, the issue often begins with PN prescription.
A broad survey of institutions revealed that only 32.7% use a computerized order entry system (CPOE) system for PN.(5) Even when CPOE is used for other medications, PN is seldom included. As in this case, most institutions still use handwritten orders requiring one or more error-prone transcription steps in the process. Available electronic health record (EHR) systems do not perform well when it comes to PN.(16) Current CPOE systems need significant improvement in nutrition support content including decision support tools. Such tools would allow for real-time alerts to any macronutrient or micronutrient dosing below or above accepted values.(5,16) Despite a number of obvious advantages over paper charts and handwritten orders, including the need for less order clarification or intervention, CPOE is of limited benefit if not built, customized, and subsequently optimized for all the users including those involved with PN.(12,17) Significantly less order clarification/intervention is required when using an electronic system compared with handwritten.(12,17)
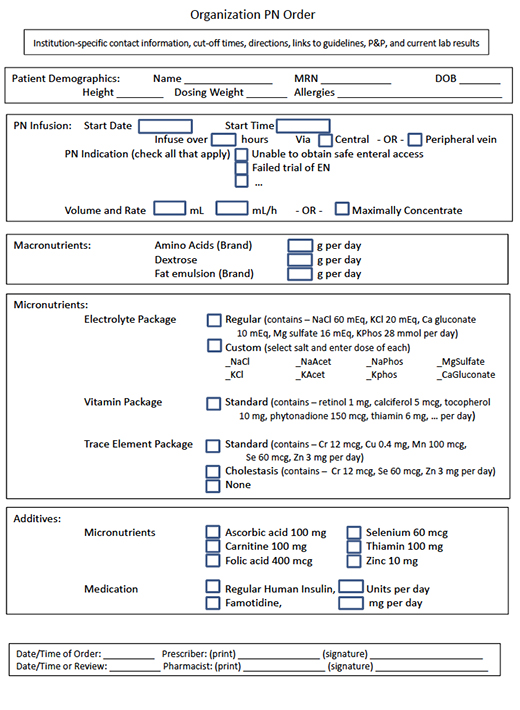
Fully integrating a CPOE system with pharmacy system can help prevent PN-related errors. Without such integration, PN should be prescribed using a standardized order template as an editable electronic document to avoid any handwritten orders (Figure). The need for any calculations or data conversion should also be avoided. Although unthinkable for most other medications, the need to specify the dose of each macronutrient and micronutrient to be included in the PN admixture varies considerably between institutions; mixed methods (mg/L for some contents, mg/kg/d for others) are sometimes even used within an institution.(4) Due to the need for weight-based dosing of nearly everything, the use of mixed methods is more likely with pediatric patients. For example, electrolytes may be ordered either by salt or by ion, as well as varying units-of-measure (e.g., mEq or mmol per kg, per L, per day, or per total volume). The ordering process should include built-in decision support and alerts for when weight-based, population-specific dosing is out of range. In the absence of built-in decision support, the critical step of pharmacist review becomes paramount. In the present case, the need to specify the dose in mg/kg/day and the need to transfer the order from a paper form to the CPOE system contributed to the error.
A survey found that 23.1% of organizations do not dedicate pharmacist time to review and clarify these orders.(5) The pharmacist should not only be trained to enter a PN order, but should be specifically knowledgeable in performing both a clinical review (e.g., dosing) and a pharmaceutical review (e.g., compatibility) of each PN order daily. Pharmacist interventions for all prescribing errors should then be documented in the permanent record. When knowledgeable pharmacists are involved, pediatric PN prescribing errors are identified and resolved at frequencies similar to those with other complex medications.(17)
Fewer than 10% of institutions have an interfaced electronic system for seamless transfer of a PN order from prescriber to pharmacy and the automated compounding device (ACD) that mixes the PN.(5) Error rates for preparing complex admixtures (including PN) are 22% to 37% depending on method of preparation.(15) ACDs are designed with the ability to provide users with alerts for dosing errors, however many institutions do not make full or appropriate use of these. Several reported PN-specific cases resulted from failure to incorporate built-in dosing limits in the ACD.(15) These limits prevent inadvertent catastrophic electrolyte doses from being included in the preparation, but require the software to be appropriate for patient age and weight. In addition to optimizing the ACD, standard operating procedures should be in place to independently double-check every step in the preparation process.
Multiple warnings occurred daily with this patient's PN order, and ignoring them contributed to the error in this case. No warning flags should be ignored or dismissed no matter whether they appear each day; each should be recognized, clarified, and documented by the pharmacist. One PN-related fatality occurred when an infant received a 1000-fold excess of zinc because of a mix-up in units and another when an infant received a 60-fold overdose of sodium.(15,18) The mix-up of dosing nutrients per kg or per day in another pediatric case was identified during PN infusion but before any adverse effect occurred.(19) When not automated, a second pharmacist should be involved in evaluating the original order against what has been transcribed, prepared, and labeled for dispensing. Some have argued that institutions should use commercially available pre-made PN formulations (not mixed from scratch at the institution). Unfortunately, commercially available pre-made PN formulations are not safer in the absence of a standardized PN-use process.(20)
The final steps in the PN-use process are administration of PN and ongoing monitoring. In this case, the nurses checked the solution against the incorrectly entered order. Instead, nurses administering PN should independently check the label against the original order. If any of the ingredients listed on the label are out of sequence or have a different dose or units than the original order, then the process should stop for clarification back up the chain through the pharmacy to the prescriber. Patient safety is worth the time it takes to verify the order. It is the responsibility of the involved prescriber, pharmacist, nurse, and dietitian to recognize and report all PN-related medication errors—whether they reach the patient or not.
The use of a CPOE system with decision support that interfaces with the pharmacy computer system thereby averting a transcription step would have prevented this patient's PN error. In the absence of such a system, required documentation of the pharmacist's review to include comparing the dose of each component against an age-appropriate table of accepted values would have also made the error less likely. Furthermore, had the nurses checked the PN label against the original order, the error may have been caught at this late step in the PN-use process.
Take-Home Points
- PN is a high-alert medication requiring safety-focused policies, procedures, and systems.
- Institutions should incorporate all appropriate ASPEN clinical guidelines and best practices documents.
- Providers should take the opportunity to enhance patient safety and reduce PN-related medication errors by becoming directly involved in the oversight of this therapy.
- Institutions should collect and report all errors associated with PN internally and externally (through the ISMP Medication Errors Reporting Program); further information is available on the ASPEN Web site.
- Providers should document each step in the PN-use process so that any errors can be evaluated and corrective actions taken to improve the process.
Joseph I. Boullata, PharmD, RPh, BCNSP
Pharmacy Specialist, Clinical Nutrition Support Services
Hospital of the University of Pennsylvania
Professor, Pharmacology & Therapeutics
University of Pennsylvania, School of Nursing
Philadelphia, PA
Faculty Disclosure: Dr. Boullata has declared that neither he, nor any immediate member of his family, have a financial arrangement or other relationship with the manufacturers of any commercial products discussed in this continuing medical education activity. In addition, the commentary does not include information regarding investigational or off-label use of pharmaceutical products or medical devices.
References
1. Boullata JI. Overview of the parenteral nutrition use process. JPEN J Parenter Enteral Nutr. 2012;36:10S-13S. [go to PubMed]
2. Andris DA, Mirtallo JM, Guenter P, eds. ASPEN parenteral nutrition safety summit. JPEN J Parenter Enteral Nutr. 2012;36(2 Suppl 2):1S-62S. [Available at]
3. ISMP's List of High-Alert Medications. Horsham, PA: Institute for Safe Medication Practices; 2012. [Available at]
4. Sacks GS, Rough S, Kudsk KA. Frequency and severity of harm of medication errors related to the parenteral nutrition process in a large university teaching hospital. Pharmacotherapy. 2009;29:966-974. [go to PubMed]
5. Boullata JI, Guenter P, Mirtallo JM. A parenteral nutrition use survey with gap analysis. JPEN J Parenter Enteral Nutr. 2013;37:212-222. [go to PubMed]
6. Sacks GS. Safety surrounding parenteral nutrition systems. JPEN J Parenter Enteral Nutr. 2012;36:20S-22S. [go to PubMed]
7. Köglmeier J, Day C, Puntis JWL. Clinical outcome in patients from a single region who were dependent on parenteral nutrition for 28 days or more. Arch Dis Child. 2008;93:300-302. [go to PubMed]
8. ISMP Medication Safety Alert! Acute Care Edition. Results of ISMP survey on high-alert medications: differences between nursing, pharmacy, and risk/quality/safety perspectives. February 9, 2012;17:1-4. [Available at]
9. Boitano M, Bojak S, McCloskey S, McCaul DS, McDonough M. Improving the safety and effectiveness of parenteral nutrition: results of a quality improvement collaboration. Nutr Clin Pract. 2010;25:663-671. [go to PubMed]
10. Mirtallo J, Canada T, Johnson D, et al; Task Force for the Revision of Safe Practices for Parenteral Nutrition. Safe practices for parenteral nutrition. JPEN J Parenter Enteral Nutr. 2004;28:S39-S70. [go to PubMed]
11. O'Neal BC, Schneider PJ, Pedersen CA, Mirtallo JM. Compliance with safe practices for preparing parenteral nutrition formulations. Am J Health Syst Pharm. 2002;59:264-269. [go to PubMed]
12. Seres D, Sacks GS, Pedersen CA, et al. Parenteral nutrition safe practices: results of the 2003 American Society for Parenteral and Enteral Nutrition survey. JPEN J Parenter Enteral Nutr. 2006;30:259-265. [Available at]
13. AHRQ Health Care Innovations Exchange. Standardized ordering and administration of total parenteral nutrition reduces errors in children's hospital. Rockville, MD: Agency for Healthcare Research and Quality; November 28, 2012. [Available at]
14. Kumpf VJ, Tillman EM. Home parenteral nutrition: safe transition from hospital to home. Nutr Clin Pract. 2012;27:749-757. [go to PubMed]
15. Cohen MR. Safe practices for compounding of parenteral nutrition. JPEN J Parenter Enteral Nutr. 2012;36(Suppl 2):14S-19S. [go to PubMed]
16. Vanek VW. Providing nutrition support in the electronic health record era: the good, the bad, and the ugly. Nutr Clin Pract. 2012;27:718-737. [go to PubMed]
17. Hilmas E, Peoples JD. Parenteral nutrition prescribing processes using computerized prescriber order entry: opportunities to improve safety. JPEN J Parenter Enteral Nutr. 2012;36(Suppl 2):32S-35S. [go to PubMed]
18. ISMP Medication Safety Alert! Acute Care Edition. Another tragic parenteral nutrition compounding error. April 21, 2011;16:1-3. [Available at]
19. ISMP Medication Safety Alert! Acute Care Edition. Mismatched prescribing and pharmacy templates for parenteral nutrition (PN) lead to data entry errors. June 28, 2012;17:1-3. [Available at]
20. Poh BY, Benjamin S, Hayward TZ III. Standardized hospital compounded parenteral nutrition formulations do not guarantee safety. Am Surg. 2011;77:e109-e111. [go to PubMed]
Figure
Figure. Electronic PN Order Form