New Patient Mistakenly Checked in as Another
Green RA, Adelman JS. New Patient Mistakenly Checked in as Another. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2016.
Green RA, Adelman JS. New Patient Mistakenly Checked in as Another. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2016.
The Case
A 55-year-old man, presented to a primary care physician's office for an initial visit to establish care and obtain routine health maintenance. He had not seen a physician in some time, but since his older brother had recently had a heart attack, he wanted to ask a physician if he should have his cholesterol checked and what else he could do to reduce his risk of heart disease.
Unknown to him, the physician he selected had another patient with the exact same first and last name, who was also 55 years of age but had a different birthday. The office receptionist was new to the practice, had not yet met most of the patients, and was struggling to become familiar with the practice's newly installed electronic medical record (EMR). She logged in and quickly found the chart of a patient with the same age and name of the patient who was registering. Assuming this must be the same patient, she checked the "new" patient in under the "old" patient's medical record number.
The physician examined the patient and advised that given his age and family history, he should have a fasting lipid panel checked. She placed an electronic order for the lab tests to be performed, and the patient had blood drawn the next day. The test results showed a slightly elevated low-density lipoprotein (LDL) cholesterol level, so the physician sent the results to the patient via the EMR's patient portal, along with a note advising him to modify his diet and engage in a weight loss program for the next 3 months.
Because of the mistake made when registering the patient, the test results and email from the physician actually went to the other patient—the one who was an established patient of the practice. When he logged into the patient portal, he was surprised, as he had not had any labs drawn recently. Moreover, he was already taking medication to reduce his cholesterol. He called the office and told them that there seemed to be a mix-up with his test results. Only then was the registration error noticed.
The Commentary
by Robert A. Green, MD, MPH, and Jason Adelman, MD, MS
Wrong-patient orders placed in an electronic health record (EHR) are common and pose a significant risk to patient safety. A 2014 report from the Office of the National Coordinator for Health Information Technology (ONC) reviewed 20,758 health information technology (IT)–related events reported to 2 large Patient Safety Organizations and concluded that "despite national efforts, wrong-patient errors were among the most common human–computer interface issues—described in 15% of all health IT–related events."(1) In this report, wrong-patient errors were noted to occur at the time of appointment scheduling, registration, and when orders were entered into the EHR system. Factors believed to contribute to wrong-patient errors include selecting the wrong record when multiple records are open at once; failing to log off the EHR system after placing orders; selecting the wrong patient when multiple patients have the same or similar names; and issues of inattention, distraction, and interruption.
As outpatient providers generally manage only one patient at a time, it may be presumed that outpatients have fewer wrong-patient errors as compared to hospital or emergency department patients. However, the opposite is true. One study demonstrated that wrong-patient errors are most common in outpatient practices; in fact, the error rate in ambulatory care is almost double that seen in the emergency department (Table 1).(2)
This case demonstrates the classic "Swiss Cheese" model of error causation. Both the patient and the receptionist were new to the practice, the patient happened to be the same age and have the same name as another patient in the practice, and the office had a newly installed EHR system. While each issue may not present a significant risk on its own, the convergence of the multiple potential failure points during registration significantly increased the risk of a wrong-patient error.
Registration is the initial point of entry for patients into a health system. It is essential that patients are properly identified at registration and that data are carefully checked and entered into the system correctly. Typos, misspellings, transpositions, and empty fields can all cause problems downstream from registration, potentially leading to wrong-patient errors. A 2008 Johns Hopkins study found that the majority of patient identification errors in the emergency department were due to errors occurring during registration.(3) A report on patient identification and matching prepared for the ONC noted that education of registration clerks is an essential step in preventing patient identification errors, but also acknowledged that such positions experience frequent turnover, making training a challenge.(4) The National Association of Healthcare Access Management (NAHAM) has a certification program for health care registration personnel, but currently there is no national requirement for certification of health care registrars.
We might expect that wrong-patient orders occur frequently in situations where providers are caring for patients with similar names. However, one study at New York-Presbyterian Hospital reviewed more than 1500 wrong-patient electronic orders and found that only 3.2% of the errors involved patients with similar sounding names.(5) The larger issue is provider distraction, as another study found that more than 80% of wrong-patient electronic orders were caused by the frequent toggling between patients coupled with numerous interruptions.(2) After an interruption, providers may forget they had switched patients prior to the interruption and place orders on the wrong patient. A Patient ID Verification Alert (e.g., displaying patient identifiers) and a Patient ID Re-Verification Function (e.g., requiring prescribers to re-enter patient identifiers prior to placing orders) have both been shown to decrease these errors.(2,6)
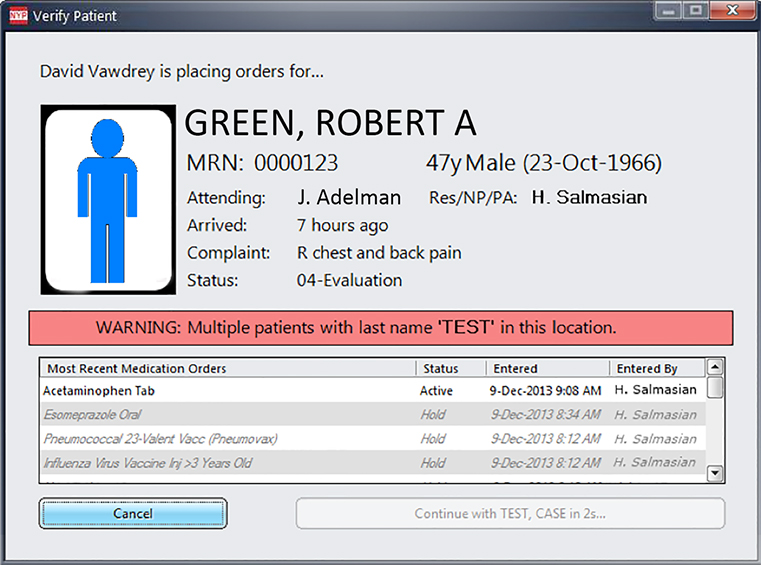
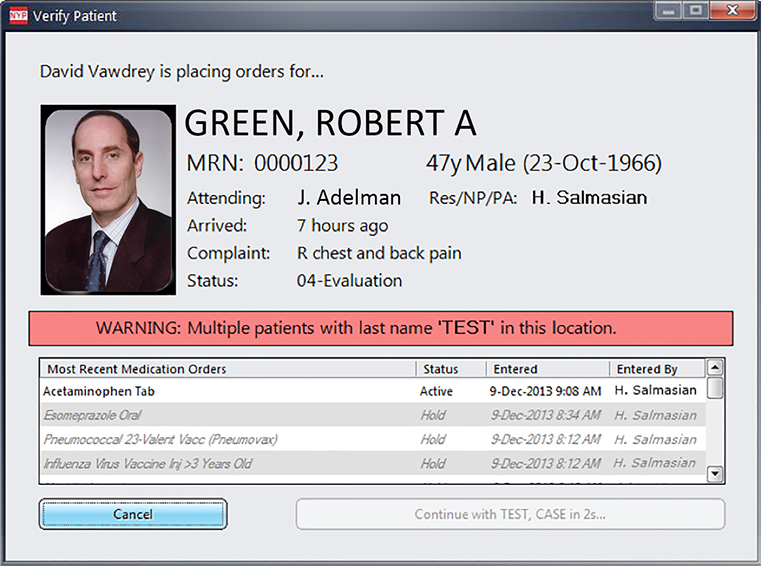
A study published in Pediatrics in 2012 demonstrated that patient photographs may be a promising strategy for reducing wrong-patient orders.(7) Although the results were encouraging, the study was restricted to inpatients and was limited by a small sample size, a quasi-experimental design, and a reliance on voluntarily reported errors. A more robust study using a rigorous research design is needed to define the true benefit of patient photographs. An ideal study will evaluate the effect of photographs for both inpatients and outpatients, as well as assess the varying ways EHR systems display patient photographs. For example, some systems display a photograph in the banner on every screen, other systems display a photograph at the time of order entry, and still other systems combine these features. The Figure provides an example of a Patient ID Verification Alert with and without a patient photograph.
In response to national concerns about health IT safety, in 2014 ONC published nine SAFER Guides designed to help health care organizations optimize the safety of their EHRs.(8) The issues that led to the error in this case are addressed by many of the recommendations in the guides (Table 2). In fact, one of these SAFER Guides is dedicated to the subject of patient identification and offers 14 specific recommendations aimed at preventing wrong-patient errors, including displaying patient photographs.(9)
In addition to the ONC SAFER Guides, many health care facilities are beginning to experiment with newer technologies such as biometric identification methods (e.g., palm scans and fingerprints), as well as patient kiosks (i.e., where patients can access and adjust their own demographic information).(4) These technologies are promising, but additional research is needed to understand their effectiveness and how they can be optimized to prevent wrong-patient errors.
Wrong-patient errors are a serious threat to patient safety. Health care facilities should strongly consider implementing the ONC SAFER Guides to conduct self-assessments of their EHR systems and workflows, follow the recommended practices that address safe use of health IT, and consider experimenting with new technologies such as identification biometrics.
Take-Home Points
- Wrong-patient orders placed in an electronic health record (EHR) are common and pose a significant risk to patient safety.
- A major cause of wrong-patient electronic orders includes providers being distracted when placing orders.
- Displaying patient photographs is a promising strategy for reducing wrong-patient orders, but more research is needed.
- In 2014, the Office of the National Coordinator for Health Information Technology (ONC) published the SAFER Guides designed to help health care organizations optimize the safety of their EHRs, and one of these guides is dedicated to the subject of patient identification.
- Many health care facilities are beginning to experiment with newer technologies to ensure proper patient identification, including the use of biometrics.
Robert A. Green, MD, MPH Vice President, Division of Quality & Patient Safety NewYork-Presbyterian Hospital
Jason Adelman, MD, MS Chief Patient Safety Officer Associate Chief Quality Officer NewYork-Presbyterian Hospital/Columbia University Medical Center Milstein Hospital
References
1. Health Information Technology Adverse Event Reporting: Analysis of Two Databases. Washington, DC: Office of the National Coordinator for Health Information Technology; November 2014. [Available at]
2. Adelman JS, Kalkut GE, Schechter CB, et al. Understanding and preventing wrong-patient electronic orders: a randomized controlled trial. J Am Med Inform Assoc. 2013;20:305-310. [go to PubMed]
3. Bittle MJ, Charache P, Wassilchalk DM. Registration-associated patient misidentification in an academic medical center: causes and corrections. Jt Comm J Qual Patient Saf. 2007;33:25-33. [go to PubMed]
4. Patient Identification and Matching: Final Report. Washington, DC: Office of the National Coordinator for Health Information Technology; February 2014. [Available at]
5. Salmasian H, Green R, Friedman C, Hripcsak G, Vawdrey D. Are patients with similar names at greater risk for wrong-patient orders? In: 2015 Summit on Clinical Research Informatics; March 23–27, 2015; San Francisco, CA. [Available at]
6. Green RA, Hripcsak G, Salmasian H, et al. Intercepting wrong-patient orders in a computerized provider order entry system. Ann Emerg Med. 2015;65:679-686. [go to PubMed]
7. Hyman D, Laire M, Redmond D, Kaplan DW. The use of patient pictures and verification screens to reduce computerized provider order entry errors. Pediatrics. 2012;130:e211-e219. [go to PubMed]
8. Sittig DF, Ash JS, Singh H. ONC issues guides for SAFER EHRs. J AHIMA. 2014;85:50-52. [go to PubMed]
9. SAFER Guides: Patient Identification. Washington, DC: Office of the National Coordinator for Health Information Technology; January 2014. [Available at]
Tables
Table 1. Wrong-Patient Errors by Visit Type.
| Wrong-patient orders per 100,000 orders | |
|---|---|
| Outpatient | 85 |
| Inpatient | 64 |
| Emergency Department | 43 |
Table 2. Examples of Recommendations From the ONC SAFER Guides That May Have Prevented the Error in This Case.
|
Figure
Figure. Examples of the NewYork-Presbyterian Patient ID Verification Alert, With and Without a Patient Photograph.