Hypoxic Gas Supply from Cross-Connected Pipelines
Bohringer C, Guemidjian A, Utter G. Hypoxic Gas Supply from Cross-Connected Pipelines. PSNet [internet]. Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2024.
Bohringer C, Guemidjian A, Utter G. Hypoxic Gas Supply from Cross-Connected Pipelines. PSNet [internet]. Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2024.
The Case
An 8-year-old boy with no significant past medical history was referred for ultrasound evaluation of neck masses. Imaging revealed a multiloculated, heterogenous lesion in the left submandibular and upper cervical area. Aspiration for cytology assessment was performed with ultrasound guidance, under inhalation anesthesia with local infiltration anesthesia of the operative site. The procedure was concluded in about 3 minutes without immediate complications.
Following the procedure, an oxygen mask was applied but both oxygen saturation and heart rate plummeted. Cardiopulmonary resuscitation (CPR) was initiated with immediate endotracheal intubation, but the patient did not respond, even after multiple doses of intravenous atropine, epinephrine, volume expanders, calcium chloride, sodium bicarbonate, and steroids. After an unrevealing physical examination and cardiology consultation, the team disconnected the patient’s oxygen tubing from the wall outlet and reconnected it to a portable oxygen cylinder, which yielded immediate improvement of oxygen saturation. The patient was transferred to the intensive care unit (ICU) on a ventilator, but the neurological examination revealed fixed and dilated pupils with no response to light or deep pain stimulation (Glasgow Coma Score 3). He remained deeply comatose with poor peripheral perfusion and episodic seizures, treated with antiepileptic medications. The patient sustained three more episodes of cardiopulmonary arrest and finally died.
The hospital’s root cause analysis revealed that the wall outlet marked for oxygen was connected to nitrous oxide. It was not clear how the gas pipes were misconnected, but this error apparently followed maintenance by an inadequately trained new employee. In addition, the anesthesia machine circuit lacked an oxygen analyzer, and the machine’s self-calibration did not check the gas source. There was some role ambiguity regarding supervision and sign-off of completed maintenance jobs, and the code team had no protocol for changing gas outlets during unsuccessful resuscitations.
The Commentary
By Christian Bohringer, MBBS, Adam Guemidjian, MD, and Garth Utter, MD
Background
Inadvertent administration of a hypoxic gas mixture to a patient frequently has lethal consequences. When oxygen is absent, anaerobic respiration very rapidly leads to lactic acidosis and cardiac arrest. Asphyxia from lack of oxygen usually results in devastating morbidity even if the patient survives the episode of hypoxemia.1
Anesthesia clinicians are very aware of the enormous risk to the patient’s life if they should inadvertently administer a hypoxic gas mixture. All anesthesia machines are therefore mandated to include a monitor for measuring the inspired oxygen concentration.2 Verifying the oxygen concentration in the gas supply from pipelines and cylinders with an oxygen analyzer is also part of the routine anesthesia machine check-out procedure at the beginning of every working day.3
The risk of inadvertently administering a hypoxic gas mixture arises principally when nitrous oxide is available for inhalational anesthesia. Nitrous oxide is delivered to the anesthesia machine via a pipeline in the wall or via a cylinder mounted on the back of the machine. In some anesthetizing locations, the gas supply originates from large cylinders mounted in the wall. Cases of inadvertently administering hypoxic gas mixtures from excessive dilution of oxygen with nitrous oxide continue to be reported in medical journals and in newspapers.4,5 Specific safety features have been developed to prevent hypoxic gas mixtures, but all of them can fail under certain circumstances.6 Deaths from recreational abuse of nitrous oxide have also been reported in the literature and the question has been raised if nitrous oxide should remain easily available for commercial applications.7
When only air and oxygen are flowing in the pipelines, the gas exiting from a wall outlet can never be hypoxic (i.e., have a partial pressure of oxygen below that in room air at sea level), even when there is an inadvertent cross-connection between the pipelines. When nitrous oxide is flowing in one of the pipelines, however, an inadvertent cross-connection between the pipelines may lead to delivering a hypoxic gas mixture to the patient. If nitrous oxide flows from an outlet that is labelled as oxygen, the patient could be exposed unintentionally to 100% nitrous oxide. When this happens, desaturation occurs very quickly. Anesthesia clinicians should suspect and rule out a hypoxic gas mixture whenever they encounter very rapid desaturation or when desaturation occurs immediately after switching a patient to a new gas supply. When a patient in this situation is connected to an anesthesia machine, the low oxygen alarm that is mandatory in new machines triggers quickly. The patient should immediately receive inhaled oxygen from a new gas supply – either room air via a bag-valve resuscitator or oxygen from a different green oxygen cylinder.
When nitrous oxide or carbon dioxide is delivered erroneously from a cylinder or a wall outlet via a non-rebreather mask, the low oxygen alarm does not trigger because the inspired oxygen concentration is not measured with this delivery system. It is therefore very important for staff to verify both the color of the cylinder as well as the identity of the gas in the cylinder before they administer the gas to the patient via a non-rebreather mask. In the United States oxygen cylinders are color-coded green, but in some other countries oxygen cylinders are white. It is critical that all staff know the color-coding system for gas cylinders in their country. If the non-rebreather mask is inadvertently connected to a blue nitrous oxide cylinder or a grey carbon dioxide cylinder, the patient may die rapidly from this error.
The diameter index safety system prevents an oxygen hose from accidentally being connected to a nitrous oxide outlet in the wall (Figure 1).
Figure 1. Diameter Index Safety System
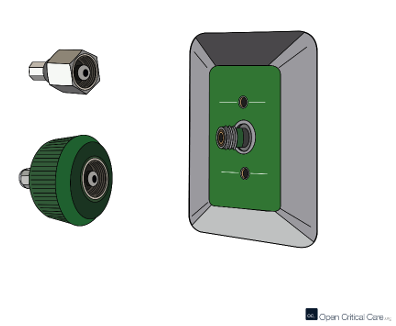
Source: Open Critical Care [Available at]
The gas hoses are also color-coded, just like the gas cylinders and the wall outlets, to prevent inadvertent cross-connection. Oxygen hoses in the United States are green and nitrous oxide hoses are blue, but the color coding for gas hoses is also not uniform internationally. Anesthesia clinicians therefore need to know the color code that is used for the hoses in the country where they are working.
Cross-connection of medical gases can also occur when cylinders are mounted in the wrong position on the anesthesia machine. The pin index safety system (Figure 2) theoretically prevents a nitrous oxide cylinder from being mounted in the location designated for an oxygen cylinder.
Figure 2. Pin Index Safety System
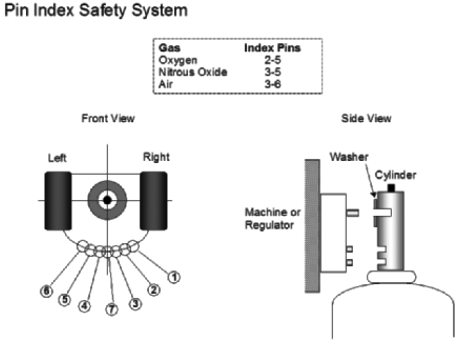
Source: Dondelinger RM. Compressed gas cylinders. Biomedical Instrumentation and Technology. 2008;42(1). [Available at]
This safety system can, however, be defeated if more than one washer is installed between the cylinder and the yoke mount on the anesthesia machine. At the beginning of the day, anesthesia professionals should therefore verify that the cylinders are mounted in the correct position by inspecting the anesthesia machine and by verifying the oxygen content of the cylinders and pipelines with an oxygen analyzer.
The flowmeters on modern anesthesia machines are mandated to have linked gas flow. When gas flow is linked, anesthesia clinicians cannot accidentally dial up a hypoxic gas mixture because oxygen is automatically increased in proportion to nitrous oxide to prevent a hypoxic gas mixture at the common gas outlet. It is very easy to accidentally administer the wrong gas by turning the wrong knob. Many procedures like endoscopies, laparoscopies and laser procedures are now performed under low ambient lighting conditions, which make it more difficult to identify the correct knob. The knob for oxygen on most anesthesia machines is bigger and has a texture that is different from the knobs for other gases, providing additional tactile feedback for the anesthesia clinician.
In some operating rooms, anesthesia machines receive their gas supply from cylinders that are mounted in the wall. With this setup, anesthesia staff cannot readily inspect the cylinders but must verify the oxygen concentration with an oxygen analyzer after turning on the flowmeters on the anesthesia machine. Fatalities have occurred when oxygen cylinders in the wall were erroneously replaced by janitorial staff with nitrous oxide cylinders. Despite the multiple safety features on anesthesia machines to prevent cross-connection, rare safety failures continue to occur.6 Many new hospitals no longer have nitrous oxide pipelines as part of their operating room infrastructure because of the high cost of constructing a separate pipeline system and the risk of administering a hypoxic gas mixture in case of a cross-connection. Significant cost savings have been realized by avoiding piped nitrous oxide.8
Clinicians have been moving away from using nitrous oxide since sevoflurane has become available. Both agents have similar blood-gas partition coefficients, which means that patients emerge from anesthesia with sevoflurane almost as quickly as with nitrous oxide. Nitrous oxide is also associated with nausea and vomiting. Hypoxemia after extubation can also occur with nitrous oxide because it lacks potency and often is administered at a percentage high enough to produce hypoxia at the alveolar level. At the end of the procedure nitrous oxide diffuses from the blood into the alveoli at a faster rate than it is exhaled by the patient. It is therefore very important that any patient who received nitrous oxide is given supplementary oxygen via a non-rebreather mask to prevent this diffusion hypoxia.9
Nitrous oxide is still used as an effective analgesic during childbirth when an epidural is contraindicated. In some countries, premixed cylinders that contain 50% oxygen and 50% nitrous oxide are available for labor analgesia. When stored at cold temperatures, the gases in these pre-mixed cylinders separate and the cylinder may then deliver a hypoxic gas mixture. Cold pre-mixed cylinders therefore should be warmed up in the upright position for 24 hours before use.10
Diagnosing cross-connection of the gas supply can be very difficult because the gas flowing from the outlet may only be hypoxic intermittently, and precise prediction of pipeline flow is impossible.11 The gas flow through the cross-connection depends on the difference in pressure between the two pipelines. Nitrous oxide only flows into the oxygen pipeline when the pressure in the nitrous line is higher than that in the oxygen line. When pressure in the oxygen line drops below that in the nitrous line, it is possible for an outlet to start delivering a hypoxic mixture even after it has passed a previous inspection. Therefore, there may be a delay in identifying an erroneous cross-connection after a “repair” has been made to the pipeline. Ongoing vigilance and clinician awareness of the potential for inadvertently delivering a hypoxic gas mixture are necessary whenever nitrous oxide is available in an anesthetizing location.
When using low flow or closed-circuit anesthesia, a hypoxic gas mixture may develop in the anesthesia circle system even when the gas mixture flowing into it has an oxygen percentage above 21%. Low flow anesthesia is used to reduce the amount of sevoflurane used during anesthesia and to prevent heat loss and drying out the respiratory epithelium. When using low flow, it is very important to increase the fraction of inspired oxygen (FIO2) to prevent a hypoxic mixture from developing in the circle system. The patient is consuming oxygen out of the circle system continuously. If the amount of oxygen delivered into the circle system is less than the amount metabolized by the patient, the oxygen concentration decreases over time. The latest generation of anesthesia machines automatically increase the FIO2 with feedback from the oxygen analyzer. The clinicians dial up the oxygen concentration they would like to deliver, and the machine adjusts the flow of oxygen automatically.12 This new system effectively prevents delivering a hypoxic gas mixture due to employing low flow anesthesia.
Approach to Improving Patient Safety
Check all new gas outlets with an oxygen analyzer
Whenever a new anesthetizing location is commissioned, all gas outlets should be checked in accordance with the National Fire Protection Association (NFPA) 99, Health Care Facilities Code Handbook,13 using an oxygen analyzer.14 Only medical gas pipeline specialists who are licensed to install these complex systems should be contracted to carry out repair work. Hospital staff who maintain the pipelines must be adequately trained and thoroughly vetted before they can be entrusted with maintenance tasks that could affect the flow of gases within the pipeline system. If an existing medical gas pipeline system has been repaired, all outlets should be checked again to ensure that no cross-connection has occurred. Recertification of the outlets should be performed by a third-party entity and by personnel who were not involved in repairing the equipment. The rules and regulations that govern this process in the United States are defined in the NFPA 99 Handbook cited above.
Anesthesia clinicians should use an oxygen analyzer to verify the identity of every gas flowing into the anesthesia circuit
At the beginning of every day prior to starting the first anesthesia case, the oxygen analyzer should be used to verify that oxygen is flowing when the oxygen flowmeter is turned on. The integrity of the linked gas flow system should also be checked. When increasing the flow of nitrous oxide, the flow of oxygen should increase automatically to prevent a hypoxic mixture.
The pressure in the oxygen and nitrous oxide pipelines as well as in the cylinders mounted on the anesthesia machine should be checked before starting the anesthetic.
Conduct routine visual inspections of cylinders and gas hoses
The cylinders mounted on the anesthesia machine and the gas hoses in the anesthetizing location should be visually assessed regularly to rule out misconnection of hoses or cylinders. Anesthesia clinicians need to know the color-coding system for medical gases in their country. In the United States, oxygen is green, nitrous oxide is blue, and carbon dioxide is grey. When connecting a patient to a cylinder via a non-rebreather mask, it is especially important to ensure that it is a green oxygen cylinder because there is no low oxygen alarm with this delivery system. Extreme caution is required when performing this seemingly simple task because only the shoulder of the cylinder may be visible if it has been inserted into a sleeve in the gurney. Many hospital staff members are not aware of the severe consequences if they inadvertently connect the non-rebreather mask to the wrong cylinder.
Consider a hypoxic gas mixture as the cause for deterioration
Most anesthesia clinicians today were trained after linked gas flow became standard on anesthesia machines. They have never seen the effect of administering a hypoxic gas mixture because cross-connection of the gas supply occurs so rarely, thanks to system engineering “fixes” like the diameter index safety system, the pin index safety system and linked gas flow, as described earlier. Young clinicians must be taught that the most characteristic clinical feature of hypoxic gas mixture is very rapid desaturation. A faulty outlet may supply a hypoxic mixture only intermittently because the flow though the cross-connection depends on the pressure difference between the pipelines. When the pressure in the oxygen pipeline drops, a gas outlet may begin to deliver a hypoxic gas mixture even after it has passed a previous inspection and has been used successfully for a previous patient.
Have a low threshold to change to a different gas supply
Whenever desaturation occurs very rapidly, or a patient has a sudden and unexpected cardiac arrest, especially after being switched to a new gas supply, a hypoxic gas mixture should be suspected. This possibility should be added to the checklist for hypoxia and cardiac arrest algorithms, in appropriate clinical settings. The patient should immediately be ventilated with a self-inflating bag valve mask resuscitator, which should be readily available at the bedside and should correct the situation rapidly. If a higher FIO2 is required, oxygen can be administered from a different green oxygen cylinder. The suspicious gas outlet should not be used again until it has been checked with an oxygen analyzer. The anesthesia team in this case unfortunately continued to attempt resuscitation of the patient with nitrous oxide, which they believed to be oxygen.
Eliminate the use of nitrous oxide from anesthesia practice
Nitrous oxide is a potent greenhouse gas; some anesthesiologists have advocated its elimination from clinical practice to protect the environment.15 Nitrous oxide is used less often since volatile agents with a similar blood gas partition coefficient, such as sevoflurane, have become available. Constructing and maintaining a separate pipeline for nitrous oxide is not only very expensive but also exposes patients to the risk of inadvertently inhaling a hypoxic gas mixture. Many recently built operating room suites therefore no longer have a pipeline for nitrous oxide. Devices designed to prevent hypoxic gas mixtures are fallible, so eliminating nitrous oxide from anesthetizing locations is the only definitive way to prevent hypoxic gas mixtures due to cross-connection in the gas supply.
Increase the FIO2 when using low fresh gas flow
Using low fresh gas flow may produce a hypoxic gas mixture in the breathing circuit. This situation is easily recognized because the low oxygen alarm will sound if the system has been set up correctly. Clinicians should increase FIO2 as they reduce fresh gas flow to prevent this problem. New anesthesia machines automatically increase the flow of oxygen during low flow anesthesia to achieve the desired FIO2 set by the anesthesia clinician. This new technology effectively eliminates the risk of a hypoxic gas mixture in the breathing system because of low flow anesthesia.
Take-Home Points
- All gas outlets need to be certified before first use and after a repair has been made to the pipeline system
- Hoses and cylinders connected to anesthesia machines should be checked to rule out cross-connection
- Gas identity should be checked every morning with an oxygen analyzer
- Clinicians should suspect hypoxic gas mixture when a patient desaturates rapidly or immediately after having changed over to a new gas supply
- The color and content of a gas cylinder needs to be carefully reviewed before connecting a patient to it
- Oxygen cylinders in the United States are green; clinicians need to know the color-code for cylinders and gas hoses in their country
- When using low flow anesthesia clinicians need to ensure adequate oxygen concentration in the breathing circuit
- Eliminating nitrous oxide from the surgical suite effectively prevents most incidents of hypoxic gas mixture
Christian Bohringer MBBS
Consulting Editor, AHRQ’s Patient Safety Network (PSNet)
Professor of Anesthesiology
Department of Anesthesiology and Pain Medicine
UC Davis Health
chbohringer@ucdavis.edu
Adam Guemidjian
Medical Student
University of California at Davis
UC Davis Health
aguemidjian@ucdavis.edu
Garth Utter MD, MSc
Consulting Editor, AHRQ’s Patient Safety Network (PSNet)
Professor of Surgery
Department of Surgery
UC Davis Health
ghutter@ucdavis.edu
References
- Gillam-Krakauer M, Gowen Jr CW. Birth Asphyxia. 2023 Aug 14. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 28613533. [Free full text]
- Fresh Gas Flow Management. American Society of Anesthesiologists. January 29, 2024. Accessed September 18, 2024. [Free full text (PDF)]
- Goneppanavar U, Prabhu M. Anaesthesia machine: checklist, hazards, scavenging. Indian J Anaesth. 2013;57(5):533-540. [Free full text]
- Bonsu AK, Stead AL. Accidental cross-connexion of oxygen and nitrous oxide in an anaesthetic machine. Anaesthesia. 1983;38(8):767-769. [Free full text]
- Gas fitter charged over 2016 nitrous oxide death of newborn at Sidney hospital. The Sydney Morning Herald. August 22, 2022. Accessed September 18, 2024. [Available at]
- Donaldson M, Donaldson D, Quarnstrom FC. Nitrous oxide-oxygen administration: when safety features no longer are safe. J Am Dent Assoc. 2012;143(2):134-143. [Available at]
- Bäckström B, Johansson B, Eriksson A. Death from nitrous oxide. J Forensic Sci. 2015;60(6):1662-1665. [Available at]
- Majeed A, Awan AM. Should pipeline nitrous oxide be discontinued in secondary care: a cost-benefit analysis. Saudi J Anaesth. 2024;18(2):194-196. [Free full text]
- Cheney FW. An early example of evidence-based medicine: hypoxemia due to nitrous oxide. Anesthesiology. 2007;106(1):186-188. [Free full text]
- Bracken A, Broughton GB, Hill DW. Safety precautions to be observed with cooled premixed gases. Br Med J. 1968;3(5620):715-716. [Free full text]
- Medical gases. Health Memorandum 02-01: Medical gas pipeline systems. Department of Health. London, UK: The Stationery Office. Accessed September 18, 2024. [Free full text]
- Aisys CS2 End-tidal Control and ecoFLOW: What’s the difference. GE HealthCare. 2023. Accessed September 18, 2024. [Free full text]
- NFPA 99, Health Care Facilities Code Handbook. 2024 ed. National Fire Protection Association; 2024.
- Mandatory Testing of Medical Gas Systems. Plumbing & Mechanical. September 1, 2004. Accessed September 18, 2024. [Free full text]
- Lehmann F, Schulz CM, Leicht D, et al. Persistent use of nitrous oxide for anaesthesia in European hospitals despite its harmfulness to the climate - how emission taxation can achieve the coupling of cost-effectiveness and climate protection: observational study. BMC Health Serv Res. 2023;23(1):1392. [Free full text]



