Despite Clues, Failed to Rescue
Ghaferi AA. Despite Clues, Failed to Rescue. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2017.
Ghaferi AA. Despite Clues, Failed to Rescue. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2017.
Case Objectives
- Define failure to rescue.
- Identify the main contributors to failure-to-rescue events.
- Appreciate the ongoing areas of scientific inquiry into the prevention of failure-to-rescue events.
- Develop a baseline understanding of human factors research.
The Case
A 72-year-old woman with a history of systolic heart failure, hypertension, and chronic kidney disease who was healthy and active at baseline was admitted for an elective dilatation and curettage for postmenopausal bleeding. Because she had relatively low blood pressures during the operation and slightly more bleeding than expected, she was admitted to the inpatient gynecology service for monitoring. A postoperative hemoglobin check showed a drop from 9.5 g/dL before the procedure to 6.8 g/dL. She was given a transfusion of two units of packed red blood cells but not evaluated by a provider.
The following morning, she complained of severe abdominal pain with nausea, which the gynecology team attributed to postoperative pain. When she had persistent severe pain later that day, her heart rate was 145 beats per minute (bpm), and she had new-onset atrial fibrillation. She was moved to a telemetry unit and cardiology was consulted. The consulting cardiology service ordered medications to control her heart rate and initiated rivaroxaban, a systemic anticoagulant, for her atrial fibrillation.
The next morning, her hemoglobin level was 7.5 g/dL and her creatinine had increased from a baseline of 2.1 mg/dL to 3.1 mg/dL. Throughout the day, her severe abdominal pain and nausea continued. At 7:00 PM, she had an episode of hematemesis (bloody vomit). Her vital signs were normal, and she was given intravenous fluids. No laboratory values were checked, and there were no urgent interventions. Despite the hematemesis, the rivaroxaban was continued.
Later that night at 2:00 AM, she had another episode of hematemesis. The gynecology resident evaluated the patient and found her to be confused and complaining of abdominal pain. Stat labs were ordered but not reviewed until the following morning. She was given intravenous fluids overnight but received no specific treatments. Laboratory results were reviewed at 6:00 AM and showed her hemoglobin had dropped to 5.8 g/dL, and her creatinine had risen to 4.5 mg/dL. Bedside evaluation revealed she was hypotensive (blood pressure 75/45 mm Hg), tachycardic (heart rate 130 bpm), and confused.
The intensive care unit (ICU) team consulted at the bedside and made plans to transfer her to the ICU. While being transferred, she had a pulseless electrical activity arrest in the setting of massive hematemesis, and she died despite maximal efforts. In the end, providers believed she likely developed mesenteric ischemia in the setting of atrial fibrillation and died from bowel ischemia and gastrointestinal bleeding.
The institution performed a multidisciplinary root cause analysis and found many specific errors that contributed to her death. The group acknowledged this case was a clear example of failure to rescue a healthy woman who underwent a simple procedure. They discussed steps to prevent such an event in the future.
The Commentary
by Amir A. Ghaferi, MD, MS
The death in this case serves as an unfortunate reminder that there is no such thing as a minor procedure in surgery. As Reason's Swiss Cheese Model of failure (1) demonstrates, major errors can occur in health care settings—including surgery—following a series of minor failures.
Every year in the United States, more than 45 million patients undergo inpatient surgical procedures.(2) Although the majority of these procedures are associated with minimal risk, at least 100,000 Americans die annually as a direct consequence of surgery.(3) Many more experience serious complications and concomitant disability. Given that many surgical deaths may be avoidable (4-9), hospitals are implementing care protocols to reduce unwanted practice variation and mandating the use of checklists and timeouts. Most institutions participate in national outcomes registries to benchmark performance and target improvement activities (10,11), and pay-for-performance programs incentivize hospitals to comply with evidence-based measures to prevent complications.(12)
Such programs focus primarily on avoiding complications in the first place. While this goal is obviously important, reducing mortality may depend as much on what happens after complications have occurred. Perioperative deaths are often the culmination of a cascade of discrete clinical events. Patients who are recovering well may experience an initial seminal complication (such as an anastomotic leak after colon surgery), followed by escalation of care (e.g., reoperation, transfer to the ICU) and additional, "domino" complications (e.g., ventilator-associated pneumonia, acute renal insufficiency). Some patients will proceed to experience irremediable complications or multisystem organ failure.
Failure-to-rescue is the failure to prevent a clinically important deterioration, such as death or permanent disability, from a complication of an underlying illness or a complication of medical care. Silber and colleagues first described failure to rescue in a 1992 study that examined hospital proficiency in managing complications after common surgical procedures.(13) Overall complication rates were influenced more by patient factors (e.g., age, comorbidities, etc.) than by hospital factors, while failure-to-rescue rates (i.e., case-fatality rates in patients with a major complication) were predominantly determined by the latter. Moreover, overall hospital mortality with surgery was primarily related to failure to rescue and only weakly correlated with complication rates. These main findings were subsequently confirmed by a 2009 study.(4) In that study, hospitals in the lowest and highest quintiles of overall mortality had virtually identical rates of major complications. In contrast, low mortality hospitals were distinguished by how well they "rescued" patients once a complication had occurred. Failure-to-rescue rates were 12.5% at low mortality hospitals versus 21.4% at high mortality hospitals (p4) These findings underscore the importance of timely recognition and management of major complications and have clear implications for strategies to reduce surgical mortality.
The concept of rescue has traditionally been associated with surgical patients and the need to identify and treat postsurgical complications effectively. This association exists as elective operations are a planned episode of care where physiological changes and deviations from "typical" recovery pathways can be anticipated. Many of the principles of rescue—early recognition, teamwork, communication, safety organizing, culture—can and do apply to medical patients who have not undergone a major operation or procedure. However, the exact means for improving rescue in this population may be different. Specifically, medical patients are a much more heterogeneous population at the time of hospitalization. For example, not every patient with congestive heart failure or patient with pneumonia is the same. Patients may have a higher acuity of illness, and physiological reserves vary widely. Nonetheless, applying similar principles of early recognition and effective management of hospital-acquired complications in medical patients is very important.
A hospital's proficiency in minimizing failure to rescue could be related to factors surrounding the ability of its staff to recognize postoperative complications and/or to take actions necessary to mitigate further complications and death. Such factors include those specific to individual providers, the clinical microsystem in which postoperative patients receive their care (i.e., hospital wards and the ICU), and the broader hospital environment. Previous research in this area has focused almost exclusively on factors in the hospital environment. For example, most studies about the effectiveness of rapid response teams describe outcomes specific to a very narrow window of the acute care episode.(14-16) They do not capture the nuances of care coordination or lack thereof immediately prior to or after an incident. Several quantitative studies evaluate staffing, rapid response teams, and other resources associated with failure-to-rescue rates.(3,17-21) In general, they find that a number of factors are associated with lower failure-to-rescue rates including: higher nurse-to-patient ratios, presence of rapid response teams, overnight physician or advanced practice provider staffing, closed ICUs with board certified intensivists, increased hospital technology capabilities, and presence of house officers. Unfortunately, many of these factors are difficult to change, require significant financial investment, and must be implemented with the entire health system in mind to reduce the risk of unintended consequences.
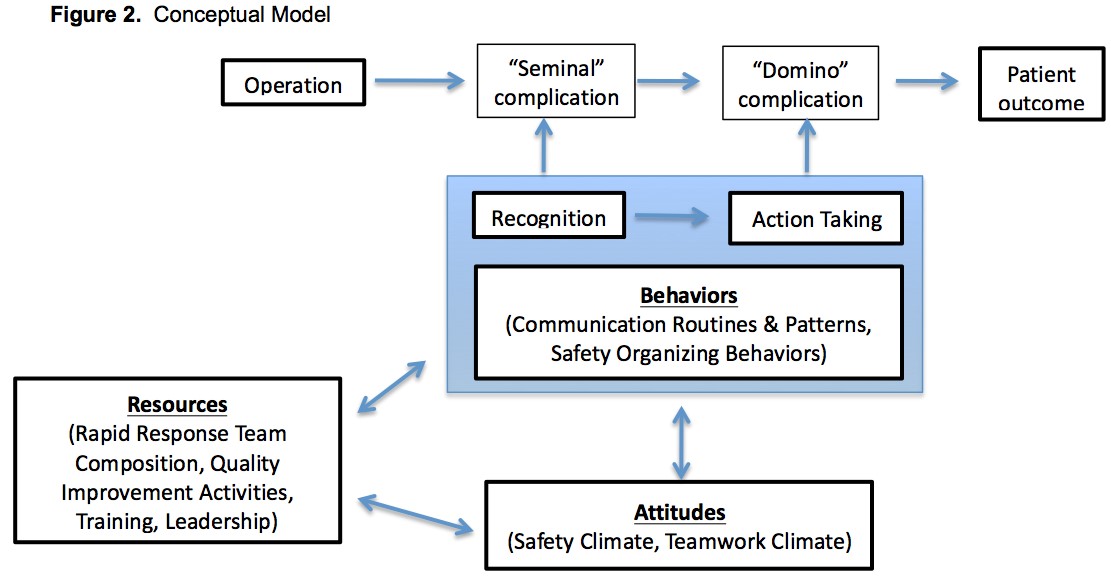
Little research has explored factors related to failure to rescue at the microsystem level. Such factors can be considered in three broad domains—resources, attitudes, and behaviors (Figure). While each of these elements can be measured crudely using existing survey methods (22,23), the important interactions between them and associated implications for designing effective interventions remain unexplored. Designing a clear, evidence-based approach that can be integrated into a health care delivery system to improve postoperative outcomes will require a focused assessment of the key elements, such as those related to effective teamwork (i.e., cooperation, trust, communication, and respect), which are critical during the "golden hours" of deterioration.
Ongoing research at the University of Michigan and Dartmouth–Hitchcock Medical Center seeks to shed light on the components that might comprise the ideal rescue system. First, researchers hope to close several important knowledge gaps in understanding variation in failure to rescue across hospitals. Most studies have focused on strategies for preventing complications, while little work has explored the determinants of failure to rescue. Research studying such factors has assessed relatively simple quantitative measures of organizational structure, resources, and culture. Focusing on very detailed, actionable aspects of teamwork and communication may provide new insight into the rescue process, and thereby enhance the ability for organizations to improve reliability.(24,25)
Although the availability of appropriate hospital and unit-level resources is vital, the structure, design, and importance of high reliability teams remains unknown. Some evidence points to environmental factors associated with effective rescue, such as nurse staffing, house officers, and ICU staffing models, but a deeper understanding of interpersonal and interdisciplinary clinical interactions is essential to inform the design and implementation of the ideal high reliability surgical team. For example, in this case the clinical staff did not seem to recognize that the patient was in distress, nor did they respond quickly and effectively to the patient's deterioration. Clinical staff's ability to both identify postoperative problems and respond appropriately may be related to the availability of resources and staffing, the safety-related behaviors of the clinical units, and/or the reliability and efficacy of team communication. A better understanding of these contributing factors is vital to designing practical and effective interventions for improving rescue.
Consensus is growing regarding the benefits of early warning scores and "smart" physiological monitoring of hospitalized patients as promising approaches to reduce failure to rescue. These approaches, along with increased staffing ratios, have long been the norm for the most critically ill patients in ICUs and have only recently been successfully applied in the general care setting. Early warning scores use risk prediction, typically generated each shift, based on vital signs and information from the electronic health record. These scores attempt to reflect patient acuity and, if accurate, could be used to adjust the setting, staffing, and monitoring used to improve patient safety. Patient surveillance in the general care setting using continuous physiological monitoring is a different but complementary approach to detect problems early and has been associated with reduced rescue events, escalation of care, and death. For example, while the naked eye can only detect major changes in physiological parameters, so-called smart monitors can utilize machine learning algorithms to detect very subtle changes in heart rate or pulse oximetry. The new signal must then be transformed into actionable information for the provider—i.e., patient exhibits signs of impending respiratory compromise, systemic inflammatory response syndrome, or sepsis.
The best approach for configuring physiologic monitors to optimally function as a safety net is unclear. Today's monitored environments are reporting so many false alarms that these systems, which are meant to alert and inform about an issue needing attention, distract the clinical team from more important activities, as discussed in a previous WebM&M commentary. In short, current systems are poorly designed, lack good user interfaces, and have not been well validated as effective in reducing failure to rescue. Researchers will continue to strive for the optimal technical design, workflow integration, and overall systems design to create a surveillance system for early detection of complications upstream in the cascade of deterioration.
While the subtleties of rescue are studied, identified, and improved, teams caring for postsurgical patients can begin to implement practical changes at the local level. First, optimizing staffing patterns is of utmost importance. This requires reevaluating the deployment of nurses and advanced practice providers to surgical wards based on acuity. There may be initial resistance to such changes whereby staff are most comfortable with the status quo, however, acuity-based staffing will provide the best chance at early recognition. Second, improving provider-to-provider communication is key. Preliminary work at the University of Michigan suggests the significant barrier to early recognition and timely action-taking is suboptimal communication between physicians and/or advanced practice providers who are making frontline management decisions. The electronic medical record is consistently cited as a barrier to effective communication given the volume of information, therefore, emphasis on traditional forms of communication (i.e., telephone or face-to-face conversations) is important.
Ultimately, avoiding inpatient deaths such as the one presented in this case will require a multipronged approach to health care system organization and design. Human factors and technology-focused solutions developed in research environments will require appropriate real-world testing, simulation, and refinement. The holy grail of patient safety may not be found in the wild, but it can certainly be forged using the ingredients put forth above.
Take-Home Points
- Failure to rescue is a failure to prevent a clinically important deterioration, such as death or permanent disability, from a complication of an underlying illness or a complication of medical care.
- Preventing failure-to-rescue events requires timely recognition of complications and appropriate action-taking by providers.
- Patient deterioration in the perioperative period may occur slowly, and early recognition requires not only medical expertise, but collaboration and communication among providers.
- Understanding the ideal methods for teamwork and communication when managing a deteriorating patient remains the focus of ongoing research.
- Avoidance of failure-to-rescue events will require a combination of human factors and technological interventions.
Amir A. Ghaferi, MD, MS Associate Professor of Surgery and Business University of Michigan Chief, Division of General Surgery, AAVA Director of Bariatric Surgery, AAVA Director, Michigan Bariatric Surgery Collaborative
Faculty Disclosure: Dr. Ghaferi has declared that neither he, nor any immediate members of his family, has a financial arrangement or other relationship with the manufacturers of any commercial products discussed in this continuing medical education activity. In addition, the commentary does not include information regarding investigational or off-label use of pharmaceutical products or medical devices.
References
1. Reason JT. Human Error. New York, NY: Cambridge: Cambridge University Press; 1990. ISBN: 9780521314190.
2. Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National Hospital Discharge Survey: 2007 summary. Natl Health Stat Report. 2010;29:1-20, 24. [go to PubMed]
3. Ghaferi AA, Osborne NH, Birkmeyer JD, Dimick JB. Hospital characteristics associated with failure to rescue from complications after pancreatectomy. J Am Coll Surg. 2010;211:325-330. [go to PubMed]
4. Ghaferi AA, Birkmeyer JD, Dimick JB. Variation in hospital mortality associated with inpatient surgery. N Engl J Med. 2009;361:1368-1375. [go to PubMed]
5. Birkmeyer JD. Improving outcomes with lung cancer surgery: selective referral or quality improvement? Ann Surg Oncol. 2009;16:1-2. [go to PubMed]
6. Birkmeyer JD, Siewers AE, Finlayson EVA, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128-1137. [go to PubMed]
7. Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117-2127. [go to PubMed]
8. Hannan EL, Kilburn H Jr, O'Donnell JF, Lukacik G, Shields EP. Adult open heart surgery in New York State. An analysis of risk factors and hospital mortality rates. JAMA. 1990;264:2768-2774. [go to PubMed]
9. O'Connor GT, Plume SK, Olmstead EM, et al. A regional prospective study of in-hospital mortality associated with coronary artery bypass grafting. The Northern New England Cardiovascular Disease Study Group. JAMA. 1991;266:803-809. [go to PubMed]
10. Fink AS, Campbell DA Jr, Mentzer RM Jr, et al. The National Surgical Quality Improvement Program in non-Veterans Administration hospitals: initial demonstration of feasibility. Ann Surg. 2002;236:344-354. [go to PubMed]
11. Hall BL, Hamilton BH, Richards K, Bilimoria KY, Cohen ME, Ko CY. Does surgical quality improve in the American College of Surgeons National Surgical Quality Improvement Program: an evaluation of all participating hospitals. Ann Surg. 2009;250:363-376. [go to PubMed]
12. Rosenthal MB, Fernandopulle R, Song HR, Landon B. Paying for quality: providers' incentives for quality improvement. Health Aff (Millwood). 2004;23:127-141. [go to PubMed]
13. Silber JH, Williams SV, Krakauer H, Schwartz JS. Hospital and patient characteristics associated with death after surgery. A study of adverse occurrence and failure to rescue. Med Care. 1992;30:615-629. [go to PubMed]
14. Karpman C, Keegan MT, Jensen JB, Bauer PR, Brown DR, Afessa B. The impact of rapid response team on outcome of patients transferred from the ward to the ICU: a single-center study. Crit Care Med. 2013;41:2284-2291. [go to PubMed]
15. Turek JW, Andersen ND, Lawson DS, et al. Outcomes before and after implementation of a pediatric rapid-response extracorporeal membrane oxygenation program. Ann Thorac Surg. 2013;95:2140-2147. [go to PubMed]
16. Beitler JR, Link N, Bails DB, Hurdle K, Chong DH. Reduction in hospital-wide mortality after implementation of a rapid response team: a long-term cohort study. Crit Care. 2011;15:R269. [go to PubMed]
17. Aiken LH, Clarke SP, Silber JH, Sloane D. Hospital nurse staffing, education, and patient mortality. LDI Issue Brief. 2003;9:1-4. [go to PubMed]
18. Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002;288:1987-1993. [go to PubMed]
19. Friese CR, Lake ET, Aiken LH, Silber JH, Sochalski J. Hospital nurse practice environments and outcomes for surgical oncology patients. Health Serv Res. 2008;43:1145-1163. [go to PubMed]
20. Pucher PH, Aggarwal R, Singh P, Darzi A. Enhancing surgical performance outcomes through process-driven care: a systematic review. World J Surg. 2014;38:1362-1373. [go to PubMed]
21. Aiken LH, Clarke SP, Cheung RB, Sloane DM, Silber JH. Educational levels of hospital nurses and surgical patient mortality. JAMA. 2003;290:1617-1623. [go to PubMed]
22. Sexton JB, Helmreich RL, Neilands TB, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res. 2006;6:44. [go to PubMed]
23. Vogus TJ, Sutcliffe KM. The Safety Organizing Scale: development and validation of a behavioral measure of safety culture in hospital nursing units. Med Care. 2007;45:46-54. [go to PubMed]
24. Ghaferi AA, Myers C, Sutcliffe KM, Pronovost PJ. The next wave of hospital innovation to make patients safer. Harv Bus Rev. July/August 2016;94. [Available at]
25. Ghaferi AA, Dimick JB. Importance of teamwork, communication and culture on failure-to-rescue in the elderly. Br J Surg. 2016;103:e45-e51. [go to PubMed]
26. Ghaferi AA, Dimick JB. Variation in mortality after high-risk cancer surgery: failure to rescue. Surg Oncol Clin N Am. 2012;21:389-395. [go to PubMed]
Figure
Figure. Conceptual Model for Understanding and Improving Failure to Rescue. Reprinted from (26) with permission from Copyright Clearance Center.