Maternal Safety
Shauer M, Nichols A, Lyndon A. Maternal Safety. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2024.
Shauer M, Nichols A, Lyndon A. Maternal Safety. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2024.
Originally published in 2018 by researchers at the University of California, San Francisco. Updated in February 2024 by Marla Shauer, PhD(c), MSN, CNM, Amy Nichols, EdD, RN, CNS, CHSE, ANEF, and Audrey Lyndon, RN, PhD, FAAN. PSNet primers are regularly reviewed and updated to ensure that they reflect current research and practice in the patient safety field.
Background
"There is no statistic that can quantify what it's like to tell an 18-month-old that his mother is never coming home." Charles Johnson
Pregnancy and birth are normal physiologic processes that optimally require support rather than medical intervention. However, the unique adaptations of pregnancy involve dramatic physiologic changes across all body systems. Many of these changes result in signs and symptoms that can make it more challenging to distinguish normal "discomforts of pregnancy" (or postpartum) from changes that would be concerning in a nonpregnant woman.
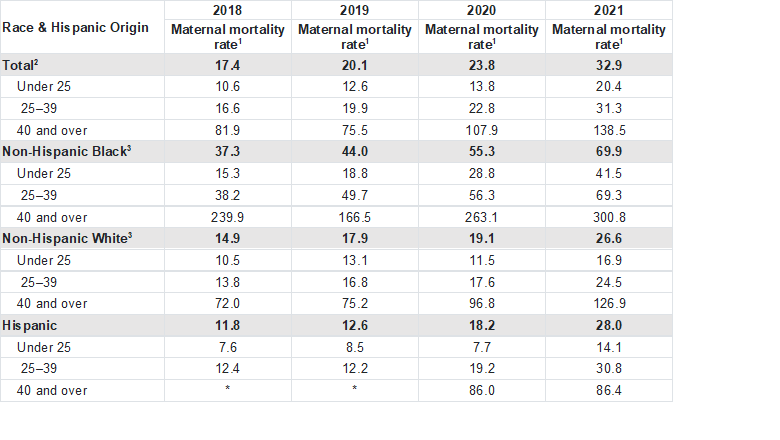
According to the Centers for Disease Control and Prevention (CDC), there were just over 3.6 million births in the United States in 2022,1 with the vast majority of births occurring in hospitals. Over 10% of the births were preterm and nearly 32% were by cesarean.2 The CDC reports 1,205 women died from maternal causes during pregnancy or within 42 days following birth.3 This reflects a US maternal mortality rate that has been rising dramatically for several years,4 from 17.4 per 100,000 live births in 2018 to 32.9 per 100,000 live births in 2021 (Table 1).3 There are substantial disparities by both racial/ethnic and socioeconomic status in maternal mortality as illustrated in Table 1. These important differences show the burden of maternal deaths is much worse in non-Hispanic Black women (69.9/100,000) compared with Hispanic women (18.0/100,000) or non-Hispanic White (26.6/100,000) women.5 Furthermore, in 2019 the CDC reported that maternal deaths between 42 days postpartum and the end of the first postpartum year account for about one-third of overall pregnancy-related deaths.5 In 2023 the CDC reported 20% of mothers who had given birth within the last 5 years reported experiencing some form of mistreatment during pregnancy or birth and almost 30% reported experiencing discrimination on the basis of race or ethnicity, age, weight, income, health insurance, or other factors.
Additionally, there are substantial disparities by racial or ethnic group or socioeconomic circumstances in pregnancy-related morbidity;6 for every maternal death, there are 70 cases of severe maternal morbidity (including unexpected outcomes of labor and delivery resulting in significant short- or long-term consequences to women’s health). As discussed in recent literature, the histories of oppression and racism in the US may be contributing to decreased health outcomes for women who have been impacted by both oppression and racism, and who may experience it as disrespect,7 or perinatal mistreatment. Women who experience discrimination also may not receive adequate information about their care, which may negatively impact their experiences of care, including worse reports of quality of care, further contributing to perinatal mistreatment and inequities during the pregnancy and postpartum periods.8,9,10 During pregnancy and birth, signs, symptoms, and women’s health concerns are often minimized or discounted by clinicians, which may further contribute to poor experiences of care. Any of these factors can lead to misdiagnosis or outright failure to recognize signs and symptoms of serious illness.
Table 1: Number of live births, maternal deaths, and maternal mortality rates, by race and Hispanic origin and age: United States, 2018–2021
Table adapted from: Hoyert DL. Health E-Stats: Maternal Mortality Rates in the United States, 2021. National Center for Health Statistics, March 2023. [Free full text]
*Rate does not meet National Center for Health Statistics standards of reliability.
1Maternal mortality rates are deaths per 100,000 live births.
2Includes deaths for race and Hispanic-origin groups not shown separately, including women of multiple races and origin not stated.
3Race groups are single race.
NOTES: Maternal causes are those assigned to code numbers A34, O00–O95, and O98–O99 of the International Classification of Diseases, 10th Revision. Maternal deaths occur while pregnant or within 42 days of being pregnant.
Patient Safety Threats and Challenges
As research evolves and begins to recognize nationally how historic structures of oppression such as racism and sexism impact groups of women in different ways, it is vital to hear the stories and threats to safety and understand how to provide consistently safe access and equitable care, for all women regardless of systemic or provider unconscious belief systems and biases.11 Pregnancy, childbirth, and the postpartum year present a complex set of safety challenges which include the negative impacts of social and structural determinants of health on birth outcomes, disparate outcomes and experiences of care, and negative experiences of care in pregnant women.11 The importance of maternal experiences and emotional harm as a threat to safety during various aspects of care are evolving as tools to measure maternal autonomy, respect and consent, or lack thereof, become available.12 Women report a variety of situations that make them feel unsafe during labor and birth such as lack of empathy and lack of agreement about care and poor communication with care providers. They can experience birth as traumatic, whether or not they have serious physical complications, and they may still report emotional, relational and/or social harm, and are at risk of avoiding care in future pregnancies.13,14,15
Labor and birth themselves are highly dynamic and situations can change rapidly. Moreover, during pregnancy, vital signs, physiologic indices, and laboratory values are altered such that findings that are “normal” for an adult can be grossly abnormal in pregnancy, labor, or postpartum and can similarly lead to failure to recognize clinical deterioration or serious illness. Thus, patients are at risk for underuse or omission if they do not receive the right care for their condition or do not receive the right care quickly enough in an emergency. Patients may also be at risk via overuse of interventions. For example, cesarean delivery rates vary widely across hospitals and providers, with the risk of liability potentially contributing to a substantial increase in use of unnecessary cesarean delivery.16 While the optimal cesarean delivery rate is unknown, the increase in cesarean delivery rates has not improved maternal or neonatal outcomes and, in fact, have contributed to maternal and infant morbidity. An example of this is the risk for infection, hemorrhage, future cesarean birth, and future potentially life-threatening placental abnormalities are greater for cesarean than for vaginal birth.17 Those who give birth by cesarean are at greater risk for severe maternal morbidity and maternal mortality,18 though the increased risk can be due to underlying conditions as well as complications from the surgery itself. Additionally, more than half of rural US counties do not have hospital-based obstetric services, significantly decreasing access for many women and families to timely care and adding to the risk for poor outcomes.19
Based on close analyses of deaths in 36 states, the CDC estimates that approximately 80% of pregnancy-related deaths in that study, or 814 of the 1,018 deaths investigated, were potentially preventable.20 This estimate is consistent with multiple studies showing that the majority (or 60-80%) of maternal deaths evaluated had at least some possible preventability, and that multiple opportunities for improvement and prevention of morbidity and mortality exist at multiple levels. In a study of the relationship between hospital birth volume and progression of severe maternal morbidity to maternal death (failure to rescue), investigators found that—after adjusting for patient characteristics and comorbidities—the hospital where the birth took place was the most important contributor to failure to rescue.21,22
Improving Patient Safety
In 1999, Knox and colleagues laid the foundation for what is now a nationwide maternal safety movement with their early application of high reliability theory to the inpatient birth setting.23 Over the past fifteen years a number of safety bundles specific to maternity care have been developed and disseminated through perinatal improvement collaboratives. This approach ultimately became a national one, through the (now dissolved) Council on Patient Safety in Women's Health Care and the Alliance for Innovation on Maternal Health (AIM). Two important facets of high reliability are standardization and effective teamwork, including "mindful interdependence." These concepts are integrated into the national and regionally developed maternal safety bundles, which are designed around the "5Rs" to enhance readiness for, recognition of, response to, and reporting (learning from) safety threats and maternal complications and providing respectful, equitable, and supportive care. AHRQ’s Safety Program for Perinatal Care (SPPC) takes an overarching approach to improving safety culture in perinatal units and is design around three pillars: teamwork and communication, perinatal safety strategies (e.g., safe electronic fetal monitoring, rapid response, medication administration) and simulation. The SPPC, AIM safety bundles, resources, implementation guides, and related education modules are freely available online (Table 2).
Table 2. Maternal Safety Bundles.
- Care for Pregnant and Postpartum People with Substance Use Disorder (AIM)
- Perinatal Mental Health Conditions (AIM)
- Cardiac Conditions in Obstetrical Care (AIM)
- Obstetric Hemorrhage (AIM)
- Postpartum Discharge Transition (AIM)
- Safe Reduction of Primary Cesarean Birth (AIM)
- Sepsis in Obstetrical Care (AIM)
- Severe Hypertension in Pregnancy (AIM)
- AHRQ Safety Program in Perinatal Care - Toolkit for Improving Perinatal Care (SPPC-I)
- AHRQ Safety Program in Perinatal Care – Toolkits to Reduce Hypertension in Pregnancy and Obstetric Hemorrhage (SPPC-II)
- Archived AIM Bundles
Maternal Toolkits
Four of the most common maternal complications which historically made the greatest contribution to maternal mortality have been targeted by the creation of toolkits specifically for these serious illnesses. These include maternal hemorrhage, preeclampsia, sepsis, and cardiac dysfunction.
ACOG defines hemorrhage as a cumulative blood loss of greater than or equal to 1,000 mL or blood loss accompanied by signs or symptoms of hypovolemia within 24 hours of a birth.24 The rate of postpartum hemorrhage rose from 2000 to 2019, from 2.7% to 4.3% (AAPC 2.6%, 94% CI 1.7-3.5%);25 it is responsible for approximately 12% of all maternal deaths.4 The Obstetric Hemorrhage toolkit (was created originally by the CMQCC in 2009) and the AHRQ SPPC Hypertension in Pregnancy and Obstetric Hemorrhage toolkit include tools to improve outcomes including patient safety bundles, evidence-based/best practice change package, data collection, and implementation support.
Preeclampsia and other hypertensive disorders of pregnancy are complex, occur on a spectrum of severity and include a wide array of disorders.26 The most severe forms can have dire consequences for both mother and infant. Preeclampsia is typically defined as a disorder of pregnancy associated with new-onset hypertension occurring after 20 weeks of gestation and frequently near term.27 The incidence of preeclampsia is estimated to occur in between 5 and 7 percent of all pregnancies, being responsible for 70,000 annual maternal deaths worldwide.27 The AIM toolkit for Severe Hypertension in Pregnancy similarly includes evidence-based/best practice change package and safety bundles and emphasizes the use of checklists and timely postpartum follow-up visits for mothers who experienced hypertension.
Maternal sepsis is defined as a life-threatening condition with organ dysfunction resulting from infection during pregnancy through 42 days postpartum.28 It is reported to be the second leading cause of maternal death in the US.28 In recent research, maternal sepsis was reported to occur in 0.04% of deliveries in the US, though 23% of maternal deaths were sepsis related.29 The AIM Sepsis in Obstetrical Care toolkit includes similar bundles and focuses on infection prevention as a key strategy.
Cardiac dysfunction is a complication referring to disorders of the cardiovascular system which may impact maternal health. The incidence of cardiac dysfunction is estimated to impact between 1% to 4% of US pregnancies and contributes with stroke to more than 34% of all pregnancy related deaths.30 These frequent maternal complications are impacted by a variety of contextual factors. The AIM Cardiac Conditions in Obstetrical Care toolkit focuses on screening for basic cardiac conditions and establishing a protocol for rapid identification of women at risk.
Current Context
With the volume of births that occur in hospitals and the high degree of preventability of hemorrhage- and hypertensive-related deaths, emergency response at birth and in the immediate postpartum period have been the focus of most maternal safety initiatives to date. However, this focus has begun to shift through strong community-based advocacy;31 increased attention from policy makers and media; and stronger recognition of the distribution of deaths across the continuum of antenatal to the full postpartum year, and the role of inequity and structural racism in producing persistent maternal health disparities.
In an effort to encourage improvements, the CDC developed State Strategies for Preventing Pregnancy-Related Deaths: A Guide for Moving Maternal Mortality Review Committee Data to Action to help organizations to move from collecting data toward a 4-step action process with each of the steps now considered through a health equity lens:
- Use data to understand the scope of the problem to identify and review complementary data to MMRC data from other population-based sources that may provide further information for identifying potential actions and associated strategies.
- Understand the context of the solutions to determine what is already being done to address the recommendation, the organizational and community factors, partnerships with key decisionmakers, and available resources (i.e., human, and financial).
- Identify potential goals and strategies based on best practices and successful examples. These goals, while not exhaustive, are illustrative and may include:
- Eliminate racial and ethnic disparities in maternal mortality.
- Invest in and partner with communities.
- Ensure access to care for all pregnant and postpartum persons.
- Ensure quality care for all pregnant and postpartum persons.
- Strengthen maternal mortality data.
- Act on your strategies, discusses important considerations for implementation, including assessing potential strategies for fit, developing an implementation plan and timeline, and planning to evaluate strategies.
Each of these steps should integrate equity, which means taking deliberate steps to value each mother’s life equally, appreciating the impact of historical trauma and institutional racism along with patient and community perspectives. Ongoing and systematic evaluation to identify facilitators and barriers to successful implementation is essential.
AHRQ has implemented and evaluated the integration of vital teamwork and communication strategies from the SPPC toolkit with two maternal safety bundles (SPPC and SPPC-II). These integrated tools include clinical case scenarios, electronic education modules, slide sets, and facilitator guidelines for AIM leaders. The California Maternal Quality Care Collaborative,32 an early developer of maternal safety bundles and implementation strategies, launched a perinatal equity collaborative to address the role of inequity and racism in birth disparities.33 Lastly, the Health Resources and Services Administration (HRSA) funds multiple initiatives to improve maternal health outcomes34 and has developed a strategic plan that highlights access to the multiple facets determined to be vital to achieving maternal safety; improving access, equity, workforce capacity, and impact.
Summary
Improving maternal safety is an ongoing challenge. It is imperative for US health care agencies and health system leaders to commit resources to improve maternal outcomes and ensure women and childbearing families experience safe, high quality, equitable, and respectful care. Greater focus on quality, safety, and equity by utilization of maternal safety tools compiled by national and state resources continues to expand capacity to improve maternal safety. Further, working within health systems to reduce diagnostic errors, preventable adverse outcomes, and serious illness are critical to improving maternal safety.
Marla Shauer, PhD(c), MSN, CNM
Health Sciences Assistant Clinical Professor
Betty Irene Moore School of Nursing
UC Davis Health
Amy Nichols, EdD, RN, CNS, CHSE, ANEF
Associate Dean for Academics
Clinical Professor
Betty Irene Moore School of Nursing
UC Davis Health
Audrey Lyndon, RN, PhD, FAAN
Vernice D. Ferguson Professor in Health Equity
Assistant Dean for Clinical Research
NYU Rory Meyers College of Nursing
References
- Martin JA, Hamilton BE, Osterman MJK. Births in the United States, 2022. NCHS Data Brief. 2023;(477):1-8. [Free full text]
- Births – Method of Delivery. Centers for Disease Control and Prevention. Accessed January 23, 2024. [Available at]
- Hoyert DL. Health E-Stats: Maternal Mortality Rates in the United States, 2021. National Center for Health Statistics, March 2023. [Free full text]
- Pregnancy Mortality Surveillance Systems. Centers for Disease Control and Prevention. Accessed January 23, 2024. [Available at]
- Petersen EE, Davis NL, Goodman D, et al. Racial/Ethnic Disparities in Pregnancy-Related Deaths - United States, 2007-2016. MMWR Morb Mortal Wkly Rep. 2019;68(35):762-765. [Free full text]
- Howell EA. Reducing disparities in severe maternal morbidity and mortality. Clin Obstet Gynecol. 2018;61(2):387-399. [Free full text]
- Green CL, Perez SL, Walker A, et al. The cycle to respectful care: a qualitative approach to the creation of an actionable framework to address maternal outcome disparities. Int J Environ Res Public Health. 2021;18(9):4933. [Free full text]
- McLemore MR, Altman MR, Cooper N, et al. Health care experiences of pregnant, birthing and postnatal women of color at risk for preterm birth. Soc Sci Med. 2018;201:127-135. [Available at
- Morton CH, Henley MM, Seacrist M, et al. Bearing witness: United States and Canadian maternity support workers' observations of disrespectful care in childbirth. Birth. 2018;45(3):263-274. [Available at]
- Howell EA, Zeitlin J. Quality of care and disparities in obstetrics. Obstet Gynecol Clin North Am. 2017;44(1):13-25. [Free full text]
- Scott KA, Britton L, McLemore MR. The ethics of perinatal care for black women: dismantling the structural racism in "Mother Blame" narratives. J Perinat Neonatal Nurs. 2019;33(2):108-115. [Free full text]
- Afulani PA, Buback L, McNally B, et al. A rapid review of available evidence to inform indicators for routine monitoring and evaluation of respectful maternity care. Glob Health Sci Pract. 2020;8(1):125-135. [Free full text]
- Attanasio LB, Hardeman RR. Declined care and discrimination during the childbirth hospitalization. Soc Sci Med. 2019;232:270-277. [Available at]
- Murphy H, Strong J. Just another ordinary bad birth? A narrative analysis of first time mothers' traumatic birth experiences. Health Care Women Int. 2018;39(6):619-643. [Available at]
- Attanasio L, Kozhimannil KB. Health care engagement and follow-up after perceived discrimination in maternity care. Med Care. 2017;55(9):830-833. [Available at]
- Kozhimannil KB, Law MR, Virnig BA. Cesarean delivery rates vary tenfold among US hospitals; reducing variation may address quality and cost issues. Health Aff (Millwood). 2013;32(3):527-535. [Free full text]
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus No. 7: Placenta Accreta Spectrum. Obstet Gynecol. 2018;132(6):e259-e275. [Available at]
- Leonard SA, Main EK, Carmichael SL. The contribution of maternal characteristics and cesarean delivery to an increasing trend of severe maternal morbidity. BMC Pregnancy Childbirth. 2019;19(1):16. [Free full text]
- Hung P, Henning-Smith CE, Casey MM, et al. Access to obstetric services in rural counties still declining, with 9 percent losing services, 2004-14 [published correction appears in Health Aff (Millwood). 2018 Apr;37(4):679]. Health Aff (Millwood). 2017;36(9):1663-1671. [Free full text]
- Trost, S, Beauregard, J, Chandra, G, et al. Pregnancy-related deaths: data from maternal mortality review committees in 36 US states, 2017-2019. Centers for Disease Control and Prevention (CDC). Accessed January 24, 2024. [Free full text]
- Friedman AM, Ananth CV, Huang Y, et al. Hospital delivery volume, severe obstetrical morbidity, and failure to rescue. Am J Obstet Gynecol. 2016;215(6):795.e1-795.e14. [Free full text]
- Lyndon A. Failure to rescue, communication, and safety Culture. Clin Obstet Gynecol. 2019;62(3):507-517. [Available at]
- Knox GE, Simpson KR, Garite TJ. High reliability perinatal units: an approach to the prevention of patient injury and medical malpractice claims. J Healthc Risk Manag. 1999;19(2):24-32. [Available at]
- Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 183: Postpartum Hemorrhage. Obstet Gynecol. 2017;130(4):e168-e186. [Available at]
- Corbetta-Rastelli CM, Friedman AM, Sobhani NC, et al. Postpartum hemorrhage trends and outcomes in the United States, 2000-2019. Obstet Gynecol. 2023;141(1):152-161. [Available at]
- Sibai BM, Lindheimer M, Hauth J, et al. Risk factors for preeclampsia, abruptio placentae, and adverse neonatal outcomes among women with chronic hypertension. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med. 1998;339(10):667-671. [Free full text]
- Preeclampsia, Genomics and Public Health. Centers for Disease Control and Prevention (CDC). Accessed January 24, 2024. [Free full text]
- Abir G, Bauer ME. Maternal sepsis update. Curr Opin Anaesthesiol. 2021;34(3):254-259. [Available at]
- Hensley MK, Bauer ME, Admon LK, et al. Incidence of maternal sepsis and sepsis-related maternal deaths in the United States. JAMA. 2019;322(9):890-892. [Free full text]
- Elkayam U, Goland S, Pieper PG, et al. High-risk cardiac disease in pregnancy: Part I. J Am Coll Cardiol. 2016;68(4):396-410. [Free full text]
- Black Mamas Matter: A Toolkit for Advancing the Human Right to Safe and Respectful Maternal Health Care. Black Mamas Matter Alliance. Accessed January 24, 2024. [Free full text]]
- California Maternal Quality Care Collaborative (CMQCC). Accessed January 24, 2024. [Free full text]]
- Cilenti D, Tissue MM, deRosset L. Developing and strengthening the current and future MCH public health workforce: building capacity, aligning systems and addressing emerging challenges. Matern Child Health J. 2022;26(Suppl 1):1-2. [Free full text]
- Perinatal Equity. California Maternal Quality Care Collaborative (CMQCC). Accessed January 24, 2024. [Free full text]