AHRQ PSNet Annual Perspective: Impact of the COVID-19 Pandemic on Patient Safety
Stocking JC, Sandrock C, Fitall E, et al. AHRQ PSNet Annual Perspective: Impact of the COVID-19 Pandemic on Patient Safety. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2021.
Stocking JC, Sandrock C, Fitall E, et al. AHRQ PSNet Annual Perspective: Impact of the COVID-19 Pandemic on Patient Safety. PSNet [internet]. Rockville (MD): Agency for Healthcare Research and Quality, US Department of Health and Human Services. 2021.
Introduction
The emergence of the COVID-19 pandemic in early 20201 had an immediate impact on everyday life. How people in the United States perform daily activities, e.g., go to work, go to school, buy their groceries, access other non-healthcare-related services, stay connected with friends and loved ones fundamentally changed, in some cases overnight. Healthcare services did not escape the unprecedented changes imposed by the COVID-19 pandemic. In the early months of the pandemic, the symptoms of the disease and details about how it was transmitted were unknown. As the numbers of cases across the country began to surge, healthcare providers, out of necessity, reduced in-person care and preserved resources by transitioning to telemedicine2 and postponing many elective procedures.3 The purpose was twofold: to reduce the burden on overwhelmed healthcare systems through increased patient surge, shortages of personal protective equipment (PPE) and ventilators, and to reduce exposure of patients at higher risk of COVID-19-related adverse outcomes to high-risk environments.
The healthcare community has come together to share insight into approaches used to prevent and reduce the spread of COVID-19, and to ensure that patients and the healthcare workforce are kept safe during the delivery of care. Researchers have also learned through disease surveillance that COVID-19 disproportionately affects racial and ethnic minority groups, particularly Latinx4 and African American populations, highlighting existing disparities in structural determinants of health5 and care. Additionally, people with behavioral health conditions, who are more likely to experience homelessness6 or incarceration,7 have a higher likelihood of exposure8 and may be more susceptible due to being disproportionately affected by comorbid medical conditions. These findings emphasize the need for bold and creative actions to address some of these underlying factors. Similarly, researchers have sought to identify ways for long-term care (LTC) facilities (including community-based group homes, board and care homes, and other congregate settings where people with disabilities and adults who are aging live)9 to protect adults who are disproportionately affected by COVID-19.10,11 Recognizing the challenges of this novel virus and the potential risks to patient safety, research in 2020 has focused on how usual care is being disrupted, how frontline providers are being affected, and the potential errors that may occur.
This Annual Perspective was developed in collaboration with Dr. Jacqueline C. Stocking, a quality improvement and critical care specialist, and Dr. Christian Sandrock, a patient safety professional and emerging infectious diseases specialist. The piece provides a look back at the evolution of the healthcare community’s understanding of COVID-19 one year after the emergence of COVID-19 in the United States. It addresses some of the most significant areas of COVID-19 patient safety news and research published in 2020 and featured on AHRQ PSNet. The observations summarize some of the lasting impacts of the COVID-19 pandemic and highlight considerations for 2021 and beyond, with a focus on areas for future research.
Impact on Usual Care
Delayed and Deferred Care
The COVID-19 pandemic has greatly impacted how healthcare is delivered. Providers and patients are navigating the use of distancing procedures and other prevention strategies aimed at minimizing risk. On the provider side, frontline staff are redesigning the delivery of care, taking into consideration the healthcare needs of the patient while also acknowledging the strains that the pandemic has put on the system.12 Healthcare institutions are faced with the difficult task of achieving a balance between the need for elective procedures and the need to protect patients and staff from COVID-19.12 Additionally, hospitals must prioritize urgent needs, such as those involving patients with cancer, to ensure that they appropriately manage their stores of PPE, and simultaneously mitigate the risks of delaying diagnosis and treatment, while also weighing the risk of virus exposure to these immunocompromised patients.
Healthcare providers and hospitals have observed a decline in patients seeking emergency care for serious medical conditions. A fear of infection has prevented patients from seeking routine medical care and screenings,13,14 and data has documented a decline in hospitalizations and a decrease in emergency department visits, with some states seeing as much as a 45% decrease in the mean number of emergency department visits per week. Further, the World Health Organization estimates that over 20 million routine preventive vaccinations will be missed due to the pandemic.15 The pandemic has also been attributed to delays in preventive cancer screenings, and ultimately diagnosis and treatment, as well as ongoing treatment of individuals with an existing cancer diagnosis.12,16,17 Delaying or deferring care can have detrimental impacts on patients by potentially worsening long-term outcomes resulting from diseases and conditions that are already diagnosed and delaying diagnosis and subsequent care for undiagnosed conditions.18,19
For a majority of patients with chronic conditions or experiencing an acute event, delaying treatment may pose a greater health risk to them than does COVID-19. A cohort study published in September 2020 found that while patients may be concerned about contracting COVID-19 in a hospital setting, it is very rare for patients to develop hospital-acquired COVID-19 when rigorous infection prevention and control measures are in place. As hospitals reopen their elective procedures and services, they need to communicate and demonstrate to patients their commitment to safety. For example, when hospitals provide patients with medical masks, require providers to also wear masks at all times, limit the number of chairs in waiting rooms, and implement physical distancing and use of plexiglass partitions, they are demonstrating to cancer patients, who are among the most at risk of adverse outcomes, their commitment to patient safety.20
Supply Shortages
Unprecedented shortages of specific supplies have created another unanticipated disruption to usual care. While shortages have not been universally experienced across the country, in locations where shortages of medications and equipment do occur, they exacerbate risks to patient care and healthcare personnel safety. In the early months of the COVID-19 pandemic, countries sought innovative alternative solutions when standard PPE was limited, notably increasing the use of reusable PPE and reusing PPE not intended for use with multiple patients (e.g., N95 masks).21,22 Similarly, as metered dose inhalers reduced the spread of COVID-19 when compared with medication delivered via nebulization, hospitals faced shortages of drugs such as asthma medications and sedatives and injectable opioids for ventilated patients.
Other Impact to Patients
In addition to impacting their usual care, the COVID-19 pandemic has exacerbated patients’ mental health challenges, particularly among young adults, racial and ethnic minority groups, essential workers, and unpaid adult caregivers.23 More than ever, patient engagement by healthcare providers is critical to ensure that patients have access to, and understand, the most accurate information available and have trust in the healthcare system. As such, the pandemic has reinforced the need for increased patient and family engagement and enhanced use of shared decision-making (SDM). Changes in the way care is delivered, through increased use of telehealth, offer providers the opportunity to consider how to improve patient management strategies, engage directly with their patients, and incorporate remote SDM.24
Impact on Providers
In Wuhan, China, where the first COVID-19 outbreak was recorded, providers reported feeling a moral and social responsibility to continue working at maximum capacity, but also expressed experiencing anxiety, distress, depression, and concerns regarding the safety of themselves and their families.25,26 Research from King’s College London and University College London has also suggested that, in England, approximately half of intensive care unit staff working through the pandemic may be suffering from mental health issues, including severe anxiety and post-traumatic stress disorder.27Clinicians in areas of the United States experiencing large outbreaks have also reported feeling stress, anxiety, and depression associated with caring for COVID-19 patients.28 Operating under these mental conditions is not only unsafe for the workforce, but also increases the potential for burnout and human error.29
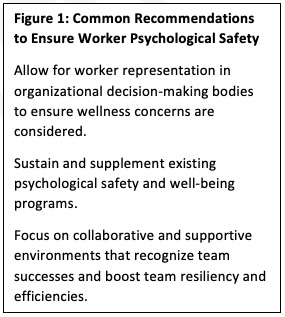
To mitigate potential negative psychological impacts on frontline staff, institutions should ensure the availability of strong infection prevention and control guidelines and effective PPE.25 Additionally, institutions can consider the implementation of strategic principles that bolster staff confidence: encouraging leadership to focus on resilience, ensuring that crisis communication provides both information and empowerment, and creating a continuum of staff support to address a surge in mental health concerns among healthcare personnel. It is also critical to understand the sources of healthcare personnel anxiety and fear in order to successfully address these emotions. Healthcare personnel would like to feel heard, protected, prepared, supported, and cared for by their organizations.30,31 An article in the New England Journal of Medicine listed five high-priority actions that can be taken at both the organizational and national level to ensure clinicians’ wellness. Separately, researchers also collated a set of evidence-based recommendations and tips to address risks to patient safety based on stressors at the level of the individual, team, and organization. In a review of recommendations for reducing workforce exposure, investigators identified a set of six core characteristics among healthcare facilities that are recommended to be included in any approach to improve practices for reducing healthcare personnel exposure. Common themes present in all of these recommended actions can be found in Figure 1. Additionally, as providers are also at high risk for substance misuse/substance use disorders, resources for prevention and recovery from substance use disorder should be included as part of medical provider support services.32
Potential Errors and Harms Associated with the COVID-19 Pandemic
Delayed or Misdiagnosis
The presence of COVID-19 in a community may increase the risk of diagnostic errors. Types of errors can include missed or delayed diagnoses in patients with respiratory problems, missed or delayed diagnosis of a non-COVID-19 condition because of the presumption that the patient has contracted COVID-19, or a missed or delayed diagnosis because of an overwhelmed health system and staff.33 Cognitive and anchoring biases in decision-making during COVID-19 are dangerous and pose a risk to patient safety. Not only can they cause providers to overlook other potential diagnoses,34 but the desire to treat may cause more harm than good, particularly when decisions are based on anecdotal information, rather than rigorous evidence-based study, as was the case in the first few months following the emergence of the virus.
Human Factors
Human factors principles address the interactions between humans and their working systems and can be helpful when trying to understand the causes of errors that result from human conditions such as stress and exhaustion. COVID-19 has the potential to introduce new patient harm events into healthcare systems and a human factors lens can be particularly useful for identifying potential error during a pandemic that has taken such a physical and emotional toll on health workers.35 One team of researchers conducted a review of cases reported to the Pennsylvania Patient Safety Reporting System to identify COVID-19-related patient safety events and found that many were associated with human factors.36 Researchers argue that adopting this human factors perspective can help to identify and prevent potential human errors.
Infection Prevention and Control
Researchers identified early in the pandemic that some frontline staff have inadequate training to correctly don and doff PPE when caring for a patient with an infectious disease, and this shortfall can greatly increase the risk of infection transmission. Infection prevention and control practices are critical components of the overall strategy to contain the spread of COVID-19 within healthcare facilities and reduce the risk of infection among healthcare personnel. However, adherence to these guidelines can be a challenge for workers, particularly during surges in the number of patients needing treatment. It is difficult for health workers to consistently comply with guidance that is complicated, ambiguous, and/or changing frequently. Additionally, a lack of support from management for workers attempting to adhere to the guidelines and a lack of available PPE can also limit the ability of well-intentioned workers to comply. Clear communication, sufficient supplies, training in the use of PPE and infection control principles and practices, and a supportive workplace safety culture all contribute to successful adherence.
Mitigating Risks of Adverse Events
Workflow Redesign
Workflow redesign has been critical to support the effectiveness of pandemic response. Not only have modifications to the workflow, particularly for inpatient settings, been instrumental in ensuring that critically ill patients receive care as safely and efficiently as possible, but they have also helped to minimize exposure outside of designated hot zones for both patients and frontline staff. The University of California, San Diego employed medical distancing to help ensure the safety of their staff. This strategy not only reduces unnecessary patient visits and unnecessary patient monitoring and socially distances providers, but it also moves equipment into the hospital hallways to limit room visits and employs “medically distanced” physical exams that are designed to reduce the number of staff that have direct contact with the patient. In addition to the increased use of telemedicine and approaches to minimize room entry, another trend among hospital medicine groups at academic medical centers is the rapid expansion of respiratory isolation units that are dedicated to patients with known or suspected COVID-19. The University of Wisconsin published a blueprint of how they restructured their Department of Surgery, focusing on changes to communication approaches to ensure regular dissemination of consistent information, reorganizing and redeploying clinical staff, and developing “strike teams” with expertise in intubation and airway management.
Primary care physicians have been able to greatly improve the safety of their workflows by moving select services from the office into the home by expanding the use of telehealth and remote patient monitoring technologies. The needs of LTC facilities vary somewhat from other inpatient facilities given the widespread vulnerabilities of their resident populations. As such, researchers have sought to identify specific recommendations unique to these facilities that will help ensure the safety of their residents. These include recommendations for establishing spaces for resident isolation, testing of residents and staff for COVID-19 infection, and resident admission to acute care hospitals.
Surge Planning
The COVID-19 pandemic has placed incredible demands on the capacity of the health system. Surge planning has become even more important for hospital operations in an effort to take into consideration and keep up with the effects of surges on staff, PPE, and other factors that determine the overall capacity of systems.37 Facilities have been faced with critical operational decisions in order to adapt and address the dynamic emergency situations at hand. Since the beginning of the pandemic, researchers have sought to review surge capacity strategies at hospitals to inform systematic recommendations for future planning, should the need for surge capacity continue.38,39 Moving forward, coordination of vaccine allocation, storage, administration, and tracking will be key components of hospital preparedness, along with managing the availability of ventilators and other critical equipment.
Role of Technology
Telehealth emerged as a critical solution to maintain continuity of some healthcare services during COVID-19, alleviating delays in care while preventing unnecessary exposure to COVID-19 for both patients and providers. Previously published Perspectives on Safety pieces have discussed the substantial expansion of services delivered through telehealth across all specialties and subspecialties, the varied experiences with telehealth across different institutions, and the associated patient safety concerns. In addition to telehealth, frontline teams are considering how electronic clinical decision support tools can better position their clinical teams for care for COVID-19 patients. For example, a team from the University of California, San Francisco created a digital tool to centralize care protocols for emergency physicians.40 The need to rigorously test tools rapidly developed for COVID-19 and other new or emerging diseases should be balanced with the urgency to identify and quickly deploy care solutions that are sorely needed. For example, artificial intelligence (AI) could be a beneficial tool to support clinical decision-making. However, there are concerns that the urgency to create AI models could result in the rapid dissemination of underdeveloped models that do not support optimal care and that have not been fully validated or evaluated. If there is bias in the data informing the AI model, the potential to inadvertently perpetuate bias against minority groups is also a risk. Before AI models can be systematically relied upon to guide treatment decisions, developers need to proactively develop comprehensive mitigation strategies to address unintended consequences.41 Moreover, with all of these technological solutions, it is important to note that small hospitals and practices may lack the financial and physical resources necessary for implementation.
Where Do We Go from Here?
Over the past year, the response of healthcare systems to the devastating impact of the COVID-19 pandemic has stimulated an increased emphasis on efforts to protect the safety of patients and healthcare personnel and on a reimagining of care delivery. The COVID-19 pandemic has served as a catalyst for some facilities to prioritize efforts such as ensuring workplace safety for care providers, facilitating the use of health IT to improve safety for both patients and providers, and strengthening the safety culture and fostering characteristics of a high-reliability organization.42 Some practices and approaches used generally by hospitals to improve safety are specifically relevant to risks and challenges posed by COVID-19. For example, tools to guide root cause analysis can help to identify breakdowns in infection control practices, including COVID-19 transmission in healthcare facilities. Researchers have developed a simple workflow chart for individuals without experience with root cause analysis to help them apply these powerful methods in nursing home facilities. In another example, researchers demonstrate the use of safety reports and Patient Family Relations complaints to implement rapid-cycle improvement to resolve safety concerns. Different delivery systems within healthcare communities are working together to respond to outbreaks, and their cooperation has generated many benefits, including an increase in the coordination of care, the use of telehealth, broader and more detailed awareness of infection prevention practices, and other foci of collaboration between historically competitive hospitals and organizations.43
Moving forward, a number of critical research priorities should be addressed as the COVID-19 pandemic continues. As identified by one scoping review, under-studied areas include supply-chain safety and occupational safety of non-healthcare essential workers. Another unanswered question is the issue of provider burnout and how providers choosing to leave the field may impact the ability of small clinics and hospitals to remain open. Additionally, it is essential to ensure that other critical patient safety efforts do not fall by the wayside. As the United States moves into the second year of the COVID-19 pandemic, patient safety researchers must consider the impact of disruptions to usual care and how the treatment of COVID-19 patients is affecting long-standing safety outcomes. For example, it is imperative to examine whether hospitals are seeing a higher rate of pressure injuries when COVID-19 patients are proning for long periods of time or are unable to move or turn when hemodynamically unstable and on a ventilator or extracorporeal life support (ECLS). It will be important to better understand the impact of COVID-19 on the rates of hospital-acquired conditions (HACs) and hospital-acquired infections (HAIs), as staff and other resources are prioritized toward critically ill COVID-19 patients and units. Additionally, reduced access to treatment for people experiencing substance use disorder may have longer-term impacts that are not yet apparent. Similarly, researchers are raising concerns about the high rate of antibiotic utilization in COVID-19 emergency department patients, despite there being no direct benefit of antibiotic use against viruses. In addition to possible setbacks in progress toward improved antibiotic stewardship, these practices also raise questions about the impact on antimicrobial resistance and rates of C. diff across the hospital. More broadly, there is a need to better understand how the response to COVID-19 has deepened healthcare disparities, exploring the impact by race, ethnicity, socioeconomic status, and also age, particularly given the critical role telehealth and technology access has played over the last year in ensuring care for individuals. Lastly, the field is just beginning to understand the burden for patients with prolonged symptoms related to COVID-19 (COVID-19 long haulers), which will further compound treatment, testing, and safety issues. Ongoing analysis of the health impacts of COVID-19 should reflect the syndromic nature of the pandemic and therefore should consider its effect on the prevalence of comorbid conditions, as well as behavioral health outcomes, such as overdose and suicide attempts.
As the country moves forward with several COVID-19 vaccines approved for emergency use, it is essential that the healthcare community and policymakers learn from past experiences to facilitate an effective and efficient nationwide vaccination program for both healthcare personnel and the general public. For example, primary care providers have historically played a critical role in vaccination programs, particularly in rural communities. Whether administering the vaccine or providing vaccination counseling services, decision makers need to consider how to better utilize these providers to support national immunization efforts. Similarly, healthcare and policy leaders must take the opportunity to assess what in the COVID-19 response at the national, state, and local level went well, identify what could have gone better, and identify and ameliorate systemic weaknesses so that all critical components of the system will be better prepared for the future, not just for medical emergencies, but also for any type of disaster that may impact healthcare systems. Failure to invest in research and evaluation that will enable this purposeful learning risks repeating the tragic consequences of the past year.
Authors
Jacqueline C. Stocking, PhD, MBA, MSN, RN, NEA-BC
Quality and Safety Analyst/Patient Safety Professional
Department of Internal Medicine
Assistant Adjunct Professor
Division of Pulmonary, Critical Care, and Sleep Medicine
University of California, Davis
Sacramento, CA
Christian Sandrock, MD, MPH, FCCP
Professor of Medicine
University of California, Davis School of Medicine
Sacramento, CA
Eleanor Fitall, MPH
Senior Research Associate, IMPAQ Health
IMPAQ International
Washington, DC
Kendall K. Hall, MD, MS
Managing Director, IMPAQ Health
IMPAQ International
Columbia, MD
Bryan Gale, MA
Senior Research Analyst, IMPAQ Health
IMPAQ International
Columbia, MD
Appendix: Published Resources
The below hyperlinks include guideline documents, recommendation statements, and other resources captured in PSNet related to the care of and/or prevention of COVID-19 that frontline healthcare personnel may find useful.
Institute for Safe Medication Practices COVID-19 Medication Safety Alert
Pain Management Best Practices During the COVID-19 Pandemic
American Geriatrics Society (AGS) Policy Brief: COVID-19 and Nursing Homes
American Geriatrics Society (AGS) Policy Brief: COVID-19 and Assisted Living Facilities
Person-Centered Guidelines for Preserving Family Presence in Challenging Times
Checklist to Facilitate Health Care Worker Disclosure of Exposure to COVID-19
Checklist to Facilitate Patient and Family Disclose of Exposure to COVID-19
Blueprint for Leadership During COVID-19
Circle Up for COVID-19 Training
References
- AJMC Staff. A timeline of COVID-19 developments in 2020. AJMC. Published January 1, 2021. Accessed February 22, 2021. https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020
- Survey: physician practice patterns changing as a result of COVID-19. Merritt Hawkins. Published April 22, 2020. Accessed July 1, 2020. https://www.merritthawkins.com/news-and-insights/media-room/press/-Physician-Practice-Patterns-Changing-as-a-Result-of-COVID-19/
- Stuart B. How the COVID-19 pandemic has affected provision of elective services: the challenges ahead. Health Affairs Blog. Published October 8, 2020. Accessed January 14, 2021. https://www.healthaffairs.org/do/10.1377/hblog20201006.263687/full/
- Double jeopardy: COVID-19 and behavioral health disparities for black and latino communities in the U.S. Substance Abuse and Mental Health Services Administration. Accessed January 11, 2021. https://www.samhsa.gov/sites/default/files/covid19-behavioral-health-disparities-black-latino-communities.pdf
- Ogedegbe G, Ravenell J, Adhikari S, et al. Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York City. Jama Netw Open.2020;3(12):e2026881. doi:10.1001/jamanetworkopen.2020.26881 [PubMed]
- Current statistics on the prevalence and characteristics of people experiencing homelessness in the united states. Substance Abuse and Mental Health Services Administration. Updated July 2011. Accessed February 24, 2021. https://www.samhsa.gov/sites/default/files/programs_campaigns/homelessness_programs_resources/hrc-factsheet-current-statistics-prevalence-characteristics-homelessness.pdf
- Aufderheide D. Mental illness in America’s jails and prisons: toward a public safety/public health model. Health Affairs Blog. Published April 1, 2014. Accessed February 24, 2021. https://www.healthaffairs.org/do/10.1377/hblog20140401.038180/full/
- COVID-19: people at increased risk. Centers for Disease Control and Prevention. Updated January 4, 2021. Accessed February 24, 2021. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/index.html
- Importance of COVID-19 vaccination for residents of long-term care facilities. Centers for Disease Control and Prevention. Published January 11, 2021. Accessed February 22, 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/LTCF-residents.html
- Gardner W, States D, Bagley N. J. The coronavirus and the risks to the elderly in long-term care. J Aging Soc Policy. 2020;32(4-5):310-315. doi: 10.1080/08959420.2020.1750543 [PSNet]
- Zimmerman S, Sloane PD, Katz PR, et al. The need to include assisted living in responding to the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21(5):572-575. doi: 10.1016/j.jamda.2020.03.024 [PSNet]
- Rosenbaum L. The untold toll — the pandemic’s effects on patients without Covid-19. New Engl J Med. 2020;382:2368-2371. doi: 10.1056/NEJMms2009984 [PSNet]
- Berstein, S. New U.S. health crisis looms as patients without COVID-19 delay care. Reuters. Published July 13, 2020. Accessed January 19, 2021. https://www.reuters.com/article/us-health-coronavirus-usa-care/new-u-s-health-crisis-looms-as-patients-without-covid-19-delay-care-idUSKCN24E143
- Czeisler MÉ, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19-related concerns--United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69(36):1250-1257. doi: 10.15585/mmwr.mm6936a4 [PSNet]
- Emergency call to action: for measles and polio outbreak prevention and response. World Health Organization. Published November 2020. Accessed November 24, 2020. https://s3.amazonaws.com/wp-agility2/measles/wp-content/uploads/2020/11/Call-To-Action-20201105.pdf
- Abdelmalek M, Bruggeman L. Dramatic drop in cancer diagnoses amid COVID pandemic is cause for concern, doctors say. ABC News. Published May 14, 2020. Accessed March 30, 2021. [PSNet]
- Stone W. Health Shots. Coronavirus strains hospitals, cancer patients face treatment delays, uncertainty. National Public Radio. Published April 2, 2020. Accessed March 30, 2021. [PSNet]
- Williams R, Jenkins DA, Ashcroft DM, et al. Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: a retrospective cohort study. The Lancet Pub Health. 2020;5(10):e543-e550. doi: 10.1016/S2468-2667(20)30201-2 [PSNet]
- Sud A, Torr B, Jones ME, et al. Effect of delays in the 2-week-wait cancer referral pathway during the COVID-19 pandemic on cancer survival in the UK: a modelling study. Lancet Oncol. 2020;21(8):1035-1044. doi: 10.1016/S1470-2045(20)30392-2 [PSNet]
- Weintraub K. 'I'm smiling under here': Masks, plexiglass and questions the norm as hospitals lure patients back in COVID-19 era. USA Today. Published June 3, 2020. Accessed March 30, 2021. [PSNet]
- Jessop ZM, Dobbs TD, Ali SR, et al. Personal protective equipment (PPE) for surgeons during COVID-19 pandemic: a systematic review of availability, usage, and rationing. Br J Surg. 2020;107(10):1262-1280. doi: 10.1002/bjs.11750 [PSNet]
- Optimizing supply of PPE and other equipment during shortages. Centers for Disease Control and Prevention. Published July 16, 2020. Accessed March 22, 2021. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/general-optimization-strategies.html
- Czeisler MÉ , Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1049–1057. DOI: http://dx.doi.org/10.15585/mmwr.mm6932a1 [PubMed]
- Abrams EM, Shaker M, Oppenheimer J, et al. The challenges and opportunities for shared decision making highlighted by COVID-19. J Allergy Clin Immunol Pract. 2020;8(8):2474-2480.e1. doi: 10.1016/j.jaip.2020.07.003 [PSNet]
- Cai H, Tu B, Ma J, et al. Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of Coronavirus Disease 2019 (COVID‑19) in Hubei, China. Med Sci Monit. 2020;26: e924171. doi: 10.12659/MSM.924171 [PSNet]
- Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. 2020;3:e203976. doi: 10.1001/jamanetworkopen.2020.3976 [PSNet]
- Greenberg N, Weston D, Hall C, et al. Mental health of staff working in intensive care during COVID-19. Occup Med (Lond). 2021;kqaa220. doi: 10.1093/occmed/kqaa220 [PubMed]
- Young KP, Kolcz DL, O’Sullivan DM, et al. Health care workers’ mental health and quality of life during COVID-19: results from a mid-pandemic, national survey. Psychiatr Serv. 2021;72(2):122-128. doi: 10.1176/appi.ps.202000424 [PubMed]
- Healthcare personnel and first responders: how to cope with stress and build resilience during the COVID-19 pandemic. Centers for Disease Control and Prevention. Updated December 16, 2020. Accessed January 11, 2021.
- Shanafelt TD, Ripp JA, Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA. 2020;323(21):2133-2134. doi: 10.1001/jama.2020.5893 [PSNet]
- Wu AW, Buckle P, Haut ER, et al. Supporting the emotional well-being of health care workers during the COVID-19 pandemic. J Patient Saf Risk Manag. 2020;25(3):93-96. doi:10.1177/2516043520931971 [PSNet]
- Addiction in medical professionals. Accessed February 24, 2021. Addiction Center. https://www.addictioncenter.com/addiction/medical-professionals/
- Khanna G, Brady J. Diagnostic safety in the COVID era: let’s not squander the opportunity. Published November 2, 2020. Accessed November 13, 2020. https://www.healthitanswers.net/diagnostic-safety-in-the-covid-era-lets-not-squander-the-opportunity/
- Brown L. COVID blindness. Diagnosis (Berl). 2020;7(2):83-84. doi: 10.1515/dx-2020-0042 [PSNet]
- Tejos R, Navia A, Cuadra A, et al. Avoiding a second wave of medical errors: the importance of human factors in the context of a pandemic. Aesthetic Plast Surg. 2020;44(5):1926-1928. doi: 10.1007/s00266-020-01868-y [PSNet]
- Taylor M, Kepner S, Gardner LA, et al. Patient safety concerns in COVID-19–related events: a study of 343 event reports from 71 hospitals in Pennsylvania. Patient Safety. 2020;2(2):16-27. doi:10.33940/data/2020.6.3 [PSNet]
- DiSilvio B, Virani A, Patel S, et al. Institutional COVID-19 protocols: focused on preparation, safety, and care consolidation. Crit Care Nurs Q. 2020;43(4):413-427. doi: 10.1097/CNQ.0000000000000327 [PSNet]
- Capolongo S, Gola M, Brambilla A, et al. COVID-19 and healthcare facilities: a decalogue of design strategies for resilient hospitals. Acta Biomed. 2020;91(9-s):50-60. doi: 10.23750/abm.v91i9-S.10117 [PSNet]
- Chopra V, Toner E, Waldhorn R, et al. How should U.S. hospitals prepare for Coronavirus disease 2019 (COVID-19)? Ann Intern Med. 2020;172(9):621-622. doi: 10.7326/M20-0907 [PSNet]
- Stark N, Kerrissey M, Grade M, et al. Streamlining care in crisis: rapid creation and implementation of a digital support tool for COVID-19. West J Emerg Med. 2020;21(5):1095-1101. doi: 10.5811/westjem.2020.7.48537 [PSNet]
- Röösli E, Rice B, Hernandez-Boussard T. Bias at warp speed: how AI may contribute to the disparities gap in the time of COVID-19. J Am Med Inform Assoc. 2021;28(1):190-192. doi: 10.1093/jamia/ocaa210 [PSNet]
- Singh H, Sittig DF, Gandhi TK. Fighting a common enemy: a catalyst to close intractable safety gaps. BMJ Qual Saf. 2021;30(2):141-145. doi: 10.1136/bmjqs-2020-011390 [PSNet]
- Wu AW, Sax H, Letaief M, et al. COVID-19: the dark side and the sunny side for patient safety. J Patient Saf Risk Manag. 2020;25(4):137-141. doi:10.1177/2516043520957116 [PSNet]